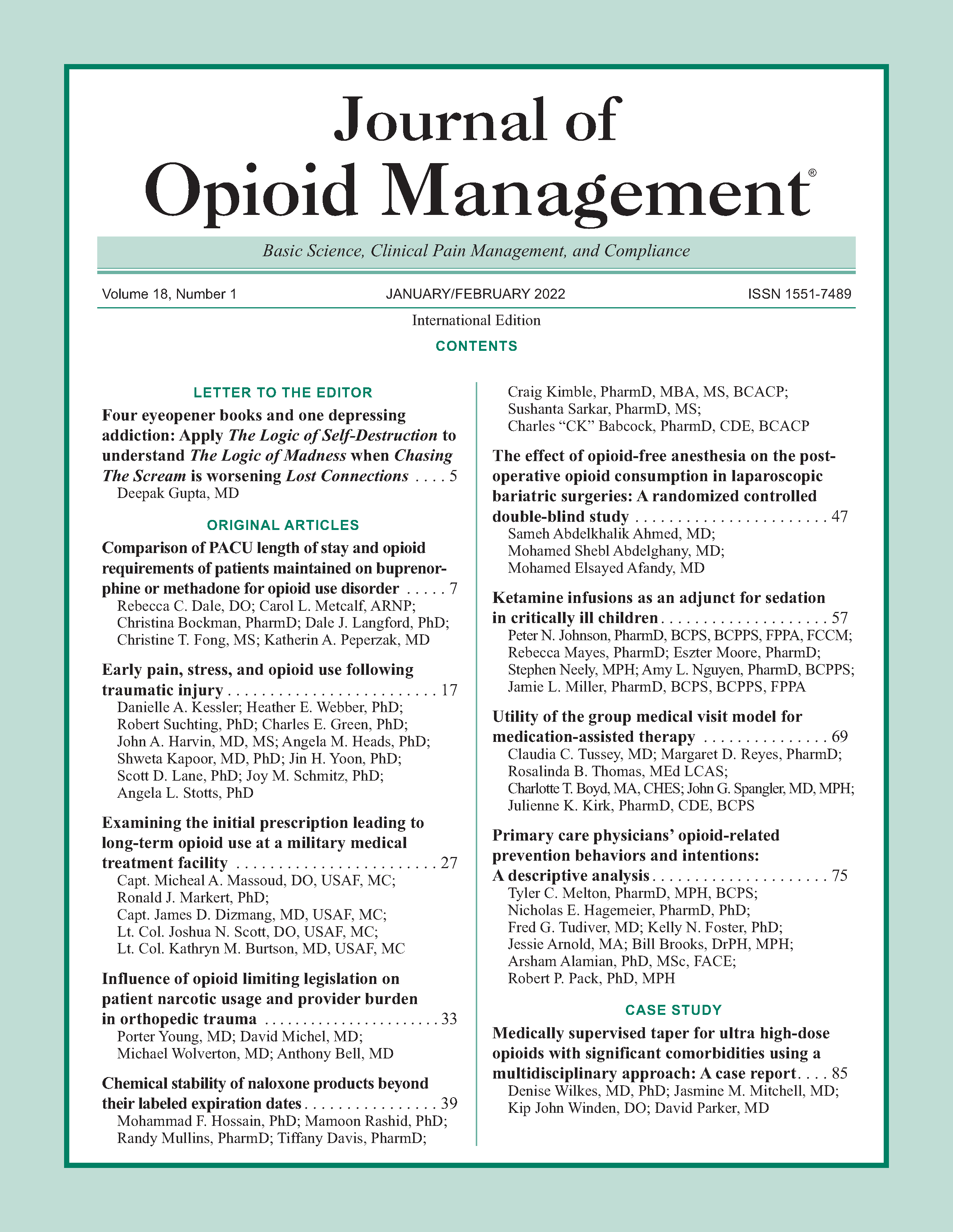
Examining the initial prescription leading to long-term opioid use at a military medical treatment facility
DOI:
https://doi.org/10.5055/jom.2022.0691Keywords:
chronic pain, initial opioid prescription, chronic opioid use, primary care, surgical subspecialtiesAbstract
Objective: Chronic pain is common in the military, and over a quarter of active-duty military members have received a prescription for opioids. This study reviewed the initial opioid prescription among those who became future long-term users at an Air Force base in the United States and reports the characteristics of the provider and patient.
Methods: Our single-center retrospective study evaluated initial opioid prescriptions leading to long-term use within the military’s electronic medical record at a large military medical treatment facility including active-duty patients and veterans. Of the 3,701 charts reviewed, 348 patients met the inclusion criteria for the long-term opioid use.
Results: Older patient groups received a higher initial amount of opioids than younger groups (p = 0.007). Primary care outpatient clinics started 43 percent of initial long-term opioid users, while surgical specialties contributed to 34 percent of the sample. In our study, 35.9 percent of the long-term opioid users were given their first opioid prescription within 30 days of an operation. Veterans or those separated from the military were less likely to have a behavioral disorder than active duty or family members.
Conclusions: Our sample mirrored the civilian population in terms of age, gender, and most common pain diagnosis. We found that older patients initially received a higher dispensed amount compared to our younger patients. There was a concerning trend for surgical patients to develop into chronic opioid users.
References
Institute of Medicine: Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press, 2011. DOI: 10.17226/13172.
Vallerand AH, Cosler P, Henningfield JE, et al.: Pain management strategies and lessons from the military: A narrative review. Pain Res Manag. 2015; 20(5): 261-268.
National Center for Health Statistics: Centers for Disease Control and Prevention. 2019. Available at https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed May 7, 2018.
Paulozzi LJ, Zhang K, Jones CM, et al.: Risk of adverse health outcomes with increasing duration and regularity of opioid therapy. J Am Board Fam Med. 2014; 27(3): 329-338.
Edlund MJ, Martin BC, Russo JE, et al.: The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: The role of opioid prescription. Clin J Pain. 2014; 30(7): 557-564.
Boudreau D, Von Korff M, Rutter CM, et al.: Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidem Drug Safe. 2009; 18(12): 1166-1175.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016; 315(15): 1624-1645. DOI: 10.1001/jama.2016.1464.
Boscarino JA, Rukstalis M, Hoffman SN, et al.: Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction. 2010; 105(10): 1776-1782.
Brummett CM, Waljee JF, Goesling J, et al.: New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017; 152(6): e170504. DOI: 10.1001/jamasurg.2017.0504.
The Washington Post/Kaiser Survey: 1 in 3 long-term prescription painkiller users think they’re addicted or dependent. Filling the need for trusted information on national health. . . . 2016. Available at http://kff.org/other/press-release/the-washington-postkaiser-survey-1-in-3-long-term-prescription-painkillerusers-think-theyre-addicted-or-dependent/. Accessed March 1, 2018.
Toblin RL, Quartana PJ, Riviere LA, et al.: Chronic pain and opioid use in US soldiers after combat deployment. JAMA Intern Med. 2014; 174(8): 1400-1401. DOI: 10.1001/jamainternmed.2014.2726.
Jeffery DD, May L, Luckey B, et al.: Use and abuse of prescribed opioids, central nervous system depressants, and stimulants among US active duty military personnel in FY 2010. Mil Med. 2014; 179(10): 1141-1148.
VA/DoD Clinical Practice Guidelines: Management for opioid therapy for chronic pain (2017)-VA/DoD clinical practice guidelines. 2009. Available at https://www.healthquality.va.gov/guidelines/Pain/cot/. Accessed March 1, 2018.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.