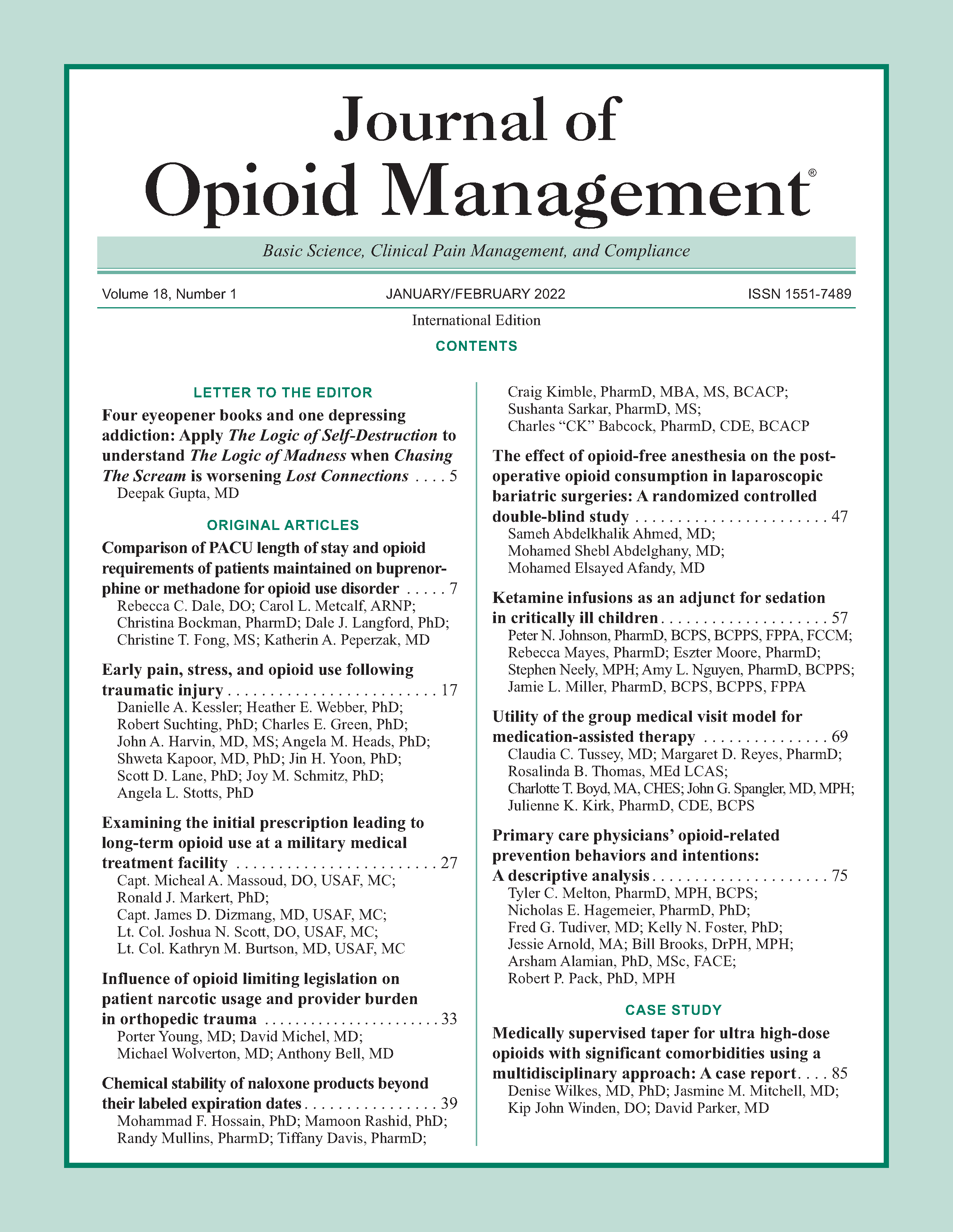
Influence of opioid limiting legislation on patient narcotic usage and provider burden in orthopedic trauma
DOI:
https://doi.org/10.5055/jom.2022.0692Keywords:
opioids, orthopedic trauma, legislationAbstract
Objective: Opiate consumption in the United States has reached alarming levels. As a result, the state of Florida enacted House Bill 21 (HB21) in July 2018. Following HB21, we hypothesized total opioids prescribed would decrease, with a resulting increase in phone calls, unscheduled visits for pain control, and refills dispensed.
Design: Retrospective cohort study comparing opiate usage 6 months before and after HB21 enactment.
Setting: Single Level I academic trauma center.
Participants: Patients with isolated lower extremity fractures who were treated with a single surgery.
Intervention: Opioid prescription limitations according to Florida's HB21.
Main outcome measures: We compared morphine milligram equivalents (MMEs) dispensed at discharge, length of stay (LOS), readmissions, emergency room (ER) visits, calls for pain control, refills, and total MMEs dispensed for 3 months postoperatively.
Results: A total of 116 patients met inclusion criteria. Our results demonstrated a decrease in the median MMEs provided at discharge (288 vs. 184, p 0.005) and total MMEs dispensed (375 vs. 225, p 0.0003). There was no significant difference in LOS (2 vs. 2.5 days, p 0.979), unscheduled clinic visits for pain (two per group), ER visits for pain (eight per group), or phone calls for pain (13 vs. 9, p 0.344). There were no readmissions for pain control pre-HB21 and one post-HB21. The percentage of patients obtaining >1 refill decreased from 22.4 to 1.7 percent (p 0.002).
Conclusions: Legislation restricting opioid pain medications may be effective in decreasing opiate use in orthopedic trauma patients while decreasing provider burden.References
Manchikanti L, Singh A: Therapeutic opioids: A ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician. 2008; 11(2 Suppl): S63-S88.
Volkow ND, McLellan TA, Cotto JH, et al.: Characteristics of opioid prescriptions in 2009. JAMA. 2011; 305(13): 1299-1301.
Blackman K, Smith E: Prescribing policies: States confront opioid overdose epidemic. 2019. Available at www.ncsl.org/research/health/prescribing-policies-states-confront-opioid-overdose-epidemic.aspx. Accessed January 1, 2020.
Fitzenhagen, Rodrigues R, Sprowls: Florida House Bill 21. Available at https://www.flsenate.gov/Session/Bill/2019/21/BillText/Filed/PDF. Accessed November 23, 2019.
Reid DBC, Shah KN, Shapiro BH, et al.: Opioid-limiting legislation associated with reduced postoperative prescribing following surgery for traumatic orthopaedic injuries. J Orthop Trauma. 2020; 34(4): e114-e120.
Reid DBC, Shah KN, Shapiro BH, et al.: Mandatory prescription limits and opioid utilization following orthopaedic surgery. J Bone Joint Surg Am. 2019; 101(10): e43.
Holman JE, Stoddard GJ, Horwitz DS, et al.: The effect of preoperative counseling on duration of postoperative opiate use in orthopaedic trauma surgery: A surgeon-based comparative cohort study. J Orthop Trauma. 2014; 28(9): 502-506.
Gangavalli A, Malige A, Terres G, et al.: Misuse of opioids in orthopaedic postoperative patients. J Orthop Trauma. 2017; 31(4): e103-e109.
Holman JE, Stoddard GJ, Higgins TF: Rates of prescription opiate use before and after injury in patients with orthopaedic trauma and the risk factors for prolonged opiate use. J Bone Joint Surg Am. 2013; 95(12): 1075-1080.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.