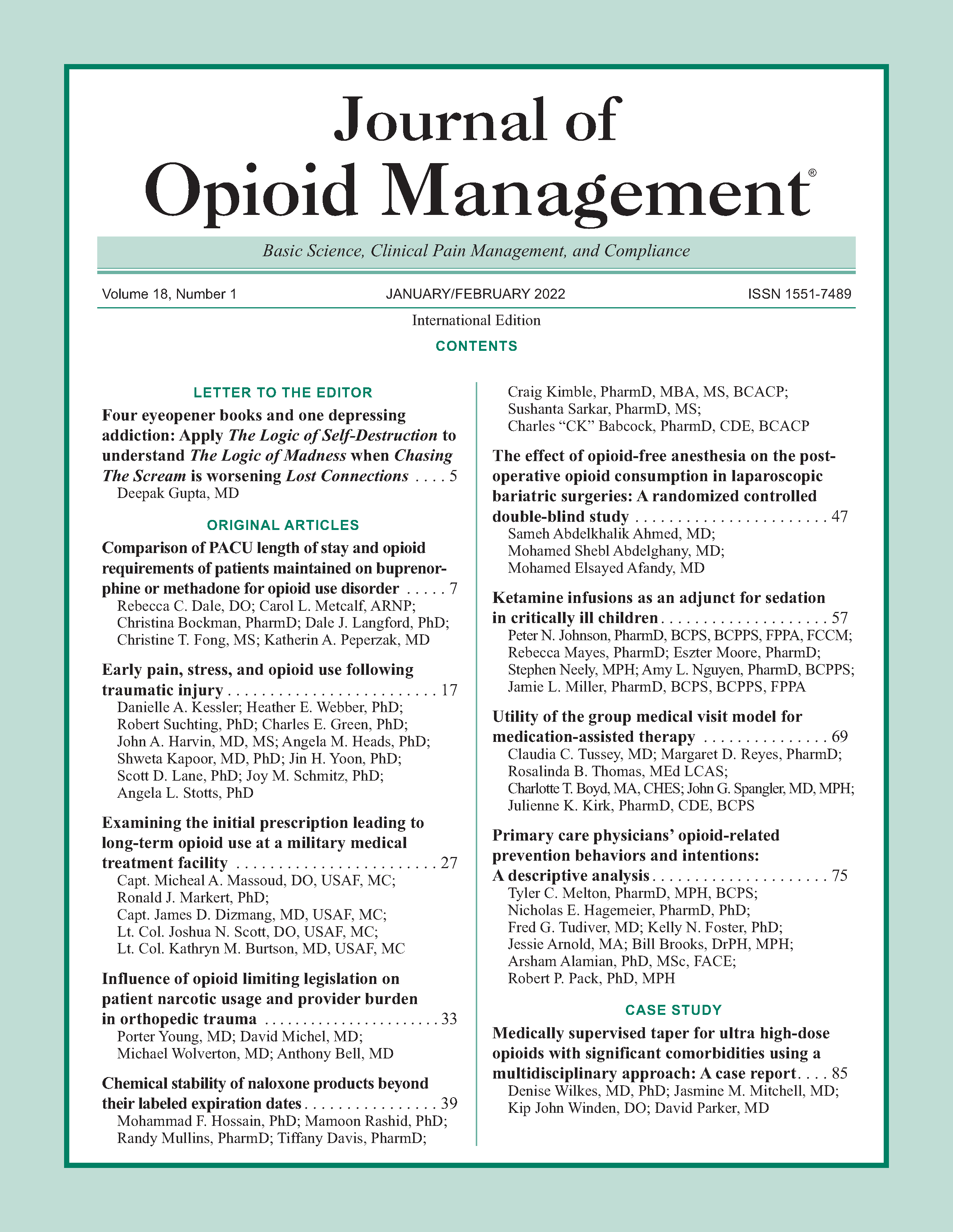
The effect of opioid-free anesthesia on the post-operative opioid consumption in laparoscopic bariatric surgeries: A randomized controlled double-blind study
DOI:
https://doi.org/10.5055/jom.2022.0694Keywords:
morphine consumption, bariatric surgery, dexmedetomidine, opioid free, nausea and vomitingAbstract
Objective: This study aimed to evaluate the ability to use opioid-free anesthesia (OFA) technique in morbid obese patients.
Design: A prospective randomized double-blinded study.
Setting: This study was carried out at Tanta University Hospitals (tertiary hospitals).
Patients: Eighty morbid obese patients scheduled for laparoscopic bariatric surgeries.
Intervention: Patients were allocated randomly into two groups: Group C, in which fentanyl was used during induction and maintenance of anesthesia, and group OFA, in which dexmedetomidine, ketamine, magnesium, and lidocaine were started before the induction of anesthesia and continued throughout the surgery.
Main outcome measure: The post-operative morphine consumption in the first 24 hours (primary outcome) and the intraoperative fentanyl consumption (secondary outcome).
Results: In comparison to the control group, OFA technique significantly decreased the post-operative morphine consumption (p = 0.003; 95 percent CI: 0.505; 2.396), shortened the time for the first request of rescue analgesia (p < 0.0001; 95 percent CI: 54.14; 99.11), decreased the post-operative pain score 4 and 6 hours after surgery (p < 0.05), and decreased the post-operative nausea and vomiting (PONV) impact scale (p = 0.022). Furthermore, it significantly decreased the intraoperative fentanyl consumption (p < 0.0001) with the improvement of all parameters of the recovery profile (p < 0.05).
Conclusion: OFA in patients undergoing bariatric surgeries significantly decreased the post-operative morphine consumption, the post-operative pain score, the intraoperative fentanyl consumption, and the PONV impact scale with the improvement of the recovery profile.
References
Kaiko R: Pharmacokinetics and pharmacodynamics of controlled-release opioids. Acta Anaesthesiol Scand. 1997; 41(1): 166-174.
Brush DE: Complications of long-term opioid therapy for management of chronic pain: The paradox of opioid-induced hyperalgesia. J Med Toxicol. 2012; 8(4): 387-392.
Gallagher SF, Haines KL, Osterlund LG, et al.: Post-operative hypoxemia: Common, undetected, and unsuspected after bariatric surgery. J Surg Res. 2010; 159(2): 622-626.
Schug SA, Raymann A: Postoperative pain management of the obese patient. Best Practice Res Clin Anaesthesiol. 2011; 25(1): 73-81.
Sultana A: Opioid free anesthesia and analgesia in the bariatric patient. Population. 2015; 8(11): 1-7.
Misiol/ek H, Zaja˛czkowska R, Daszkiewicz A, et al.: Post-operative pain management—2018 consensus statement of the section of regional anaesthesia and pain therapy of the polish society of anaesthesiology and intensive therapy, the polish society of regional anaesthesia and pain therapy, the polish association for the study of pain and the national consultant in anaesthesiology and intensive therapy. Anaesthesiol Intensive Ther. 2018; 3: 50.
Mantz J, Josserand J, Hamada S: Dexmedetomidine: New insights. Eur J Anaesthesiol. 2011; 28(1): 3-6.
Laulin J-P, Maurette P, Corcuff J-B, et al.: The role of ketamine in preventing fentanyl-induced hyperalgesia and subsequent acute morphine tolerance. Anesth Analg. 2002; 94(5): 1263-1269.
De Oliveira GS, Duncan K, Fitzgerald P, et al.: Systemic lidocaine to improve quality of recovery after laparoscopic bariatric surgery: A randomized double-blinded placebo-controlled trial. Obes Surg. 2014; 24(2): 212-218.
Levaux C, Bonhomme V, Dewandre P-Y, et al.: Effect of intra-operative magnesium sulphate on pain relief and patient comfort after major lumbar orthopaedic surgery. Anaesthesia. 2003; 58(2): 131-135.
Myles PS, Wengritzky R: Simplified postoperative nausea and vomiting impact scale for audit and post-discharge review. Br J Anaesth. 2012; 108(3): 423-429.
Cohen LB, DeLegge MH, Aisenberg J, et al.: AGA institute review of endoscopic sedation. Gastroenterology. 2007; 133(2): 675-701.
Gupta K, Prasad A, Nagappa M, et al.: Risk factors for opioid-induced respiratory depression and failure to rescue: A review. Curr Opin Anaesthesiol. 2018; 31(1): 110-119.
Hofer RE, Sprung J, Sarr MG, et al.: Anesthesia for a patient with morbid obesity using dexmedetomidine without narcotics. Can J Anesth/J Can Anesth. 2005; 52(2): 176-180.
Candiotti KA, Bergese SD, Bokesch PM, et al.: Monitored anesthesia care with dexmedetomidine: A prospective, randomized, double-blind, multicenter trial. Anesth Analg. 2010; 110(1): 47-56.
Kawasaki T, Ogata M, Kawasaki C, et al.: Ketamine suppresses proinflammatory cytokine production in human whole blood in vitro. Anesth Analg. 1999; 89(3): 665-669.
Feld JM, Laurito CE, Beckerman M, et al.: Non-opioid analgesia improves pain relief and decreases sedation after gastric bypass surgery. Can J Anesth/J Can Anesth. 2003; 50(4): 336-341.
Weinberg L, Peake B, Tan C, et al.: Pharmacokinetics and pharmacodynamics of lignocaine: A review. WJA. 2015; 4(2): 17-29.
Dabbagh A, Elyasi H, Razavi S, et al.: Intravenous magnesium sulfate for post-operative pain in patients undergoing lower limb orthopedic surgery. Acta Anaesthesiol Scand. 2009; 53(8): 1088-1091.
Seyhan T, Tugrul M, Sungur M, et al.: Effects of three different dose regimens of magnesium on propofol requirements, haemodynamic variables and postoperative pain relief in gynaecological surgery. Br J Anaesth. 2006; 96(2): 247-252.
Guinot P-G, Spitz A, Berthoud V, et al.: Effect of opioid-free anaesthesia on post-operative period in cardiac surgery: A retrospective matched case-control study. BMC Anesthesiol. 2019; 19(1): 136.
Lam KK, Mui WL: Multimodal analgesia model to achieve low postoperative opioid requirement following bariatric surgery. Hong Kong Med J. 2016; 22(5): 428-434.
Mansour MA, Mahmoud AAA, Geddawy M: Nonopioid versus opioid based general anesthesia technique for bariatric surgery: A randomized double-blind study. Saudi J Anaesth. 2013; 7(4): 387.
Bakhamees HS, El-Halafawy YM, El-Kerdawy HM, et al.: Effects of dexmedetomidine in morbidly obese patients undergoing laparoscopic gastric bypass. Middle East J Anesthesiol. 2007; 19(3): 537-551.
Vaughns JD, Martin C, Nelson J, et al.: Dexmedetomidine as an adjuvant for perioperative pain management in adolescents undergoing bariatric surgery: An observational cohort study. J Pediatr Surg. 2017; 52(11): 1787-1790.
Ziemann-Gimmel P, Goldfarb A, Koppman J, et al.: Opioid-free total intravenous anaesthesia reduces postoperative nausea and vomiting in bariatric surgery beyond triple prophylaxis. Br J Anaesth. 2014; 112(5): 906-911.
Bakan M, Umutoglu T, Topuz U, et al.: Opioid-free total intravenous anesthesia with propofol, dexmedetomidine and lidocaine infusions for laparoscopic cholecystectomy: A prospective, randomized, double-blinded study. Rev Bras Anestesiol. 2015; 65(3): 191-199.
Beloeil H, Laviolle B, Ménard C, et al.: POFA trial study protocol: A multicentre, double-blind, randomised, controlled clinical trial comparing opioid-free versus opioid anaesthesia on postoperative opioid-related adverse events after major or intermediate non-cardiac surgery. BMJ Open. 2018; 8(6): e020873.
Singh PM, Panwar R, Borle A, et al.: Perioperative analgesic profile of dexmedetomidine infusions in morbidly obese undergoing bariatric surgery: A meta-analysis and trial sequential analysis. Surg Obesity Related Dis. 2017; 13(8): 1434-1446.
Mulier JP, Dillemans B: Anaesthetic factors affecting outcome after bariatric surgery, a retrospective levelled regression analysis. Obes Surg. 2019; 29(6): 1841-1850.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.