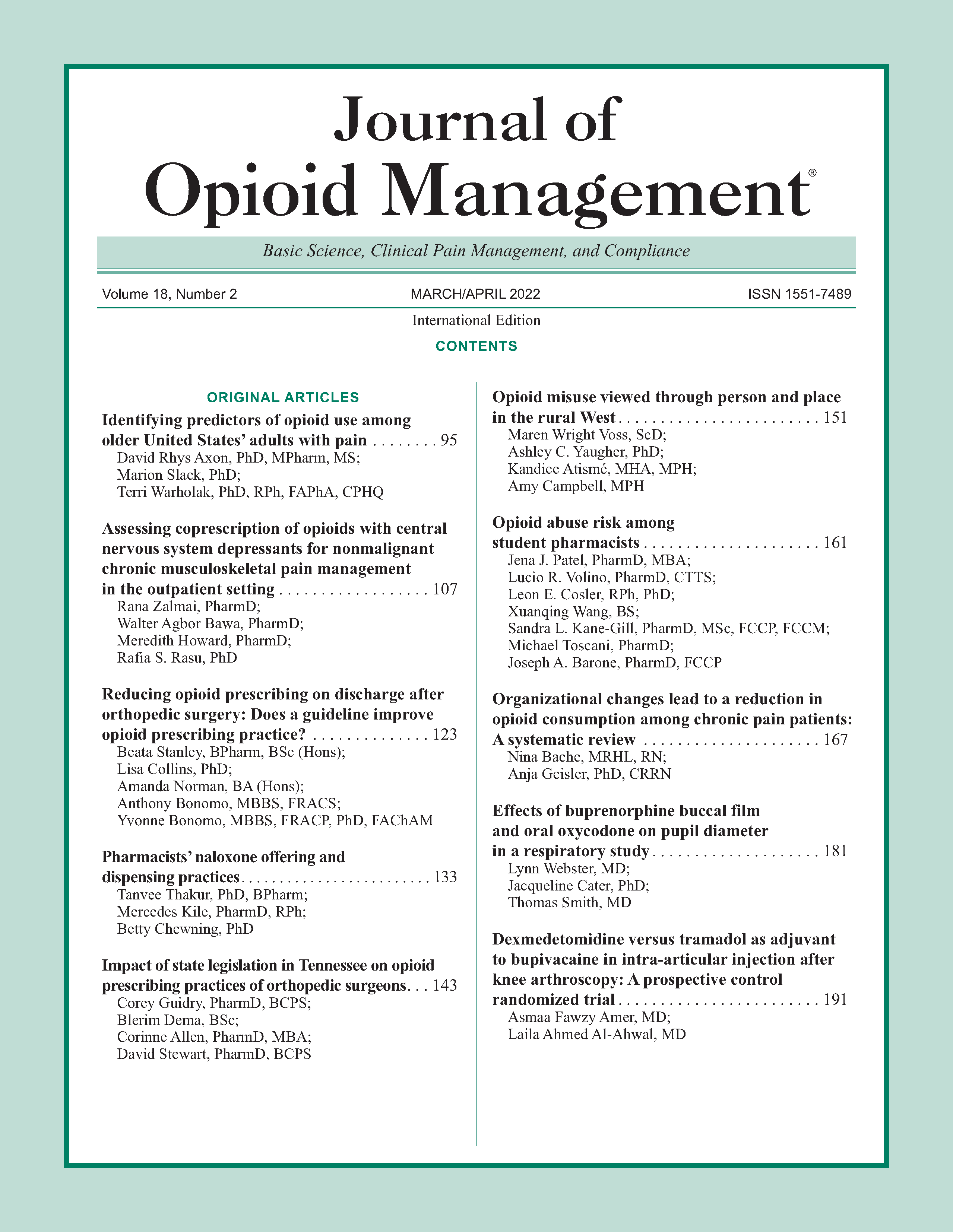
Assessing coprescription of opioids with central nervous system depressants for nonmalignant chronic musculoskeletal pain management in the outpatient setting
DOI:
https://doi.org/10.5055/jom.2022.0701Keywords:
musculoskeletal chronic pain, opioid, benzodiazepine, sedative, gabapentinoidsAbstract
Objectives: To determine annual prescribing trends of opioids and coprescription of central nervous system (CNS) depressants in nonmalignant chronic musculoskeletal pain from the National Ambulatory Medical Care Survey (NAMCS). To determine patient and provider characteristics associated with coprescription opioids and CNS depressants.
Design: The cross-sectional study analyzed NAMCS data from 2014 to 2016. Pain medications and CNS depressants were determined using Multum drug classification categories. All 30 medication entries were scanned in order to capture the maximum number of entries compared to previous studies. Multivariate logistic regressions were used to determine characteristics associated with opioid and CNS depressant coprescribing.
Participants: Adults (18 years and older) with nonmalignant chronic musculoskeletal pain diagnosis based on ICD-9 codes were identified as the reason for visit.
Results: A total of 47,973,413 weighted visits with nonmalignant chronic musculoskeletal pain were reported in the US ambulatory setting from 2014 to 2016. Amongst these patients, 31 percent were on opioids, of which 26 percent were also prescribed benzodiazepines, 8 percent NBSH, and 22 percent gabapentinoids. The annual prescribing rate of opioids decreased significantly in 2016 compared to 2014 (OR: 0.63, 95 percent CI: 0.43-0.94). Polypharmacy and tobacco use were associated with higher odds of having opioids and concurrent opioid with CNS depressants.
Conclusion: Our study results are in agreement with previous studies that found a steady decline in opioid prescribing even with the inclusion of all 30 medications in our study. Likewise, as previous studies have found, certain patient characteristics continue to be significant for receiving opioid and CNS depressant prescriptions.
References
Opioid Overdose Crisis National Institute on Drug Abuse. Available at https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis. Updated April 2020. Accessed March 3, 2020.
Bredemeyer M: CDC develops guideline for opioid prescribing. Am Fam Physician. 2016; 93(12): 1042.
NIDA: Prescription Opioids. Available at https://www.drugabuse.gov/publications/drugfacts/prescription-opioids. Published 2019. Updated June 27, 2019. Accessed February 3, 2020.
NIDA: Benzodiazepines and Opioids. Available at https://www.drugabuse.gov/drugs-abuse/opioids/benzodiazepinesopioids. Published 2019. Accessed March 15, 2018.
NIDA: Misuse of Prescription Drugs. Available at https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs. Updated December 13, 2018. Accessed April 3, 2020.
SAMHSA: Alternate Approaches to Chronic Pain [Fact sheet]. Available at https://www.samhsa.gov/sites/default/files/programs_campaigns/wellness_initiative/paw-opioid-prevention-fact-sheet.pdf. Published 2017. Updated 2017. Accessed February 11, 2019.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016; 315(15): 1624-1645.
Arnold N: FDA in Brief: FDA requires new warnings for gabapentioids about risk of respiratory depression. Updated December 12, 2019. Accessed February 24, 2020.
Dunn KM, Saunders KW, Rutter CM, et al.: Opioid prescriptions for chronic pain and overdose: A cohort study. Ann Intern Med. 2010; 152(2): 85-92.
Jann M, Kennedy WK, Lopez G: Benzodiazepines: A major component in unintentional prescription drug overdoses with opioid analgesics. J Pharm Pract. 2014; 27(1): 5-16.
Park TW, Saitz R, Ganoczy D, et al.: Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: Case-cohort study. BMJ. 2015; 350: h2698.
US Opioid Prescribing Rate Maps: Centers for Disease Control and Prevention. Updated March 5, 2020. Accessed May 5, 2020.
Bohnert ASB, Guy GP Jr, Losby JL: Opioid prescribing in the United States before and after the centers for disease control and prevention's 2016 opioid guideline. Ann Intern Med. 2018; 169(6): 367-375.
Deyo RA, Smith DH, Johnson ES, et al.: Opioids for back pain patients: Primary care prescribing patterns and use of services. J Am Board Fam Med. 2011; 24(6): 717-727.
Rhee TG: Coprescribing of benzodiazepines and opioids in older adults: Rates, correlates, and national trends. J Gerontol A Biol Sci Med Sci. 2019; 74(12): 1910-1915.
Ladapo JA, Larochelle MR, Chen A, et al.: Physician prescribing of opioids to patients at increased risk of overdose from benzodiazepine use in the United States. JAMA Psychiatry. 2018; 75(6): 623-630.
Hirschtritt ME, Delucchi KL, Olfson M: Outpatient, combined use of opioid and benzodiazepine medications in the United States, 1993-2014. Prev Med Rep. 2018; 9: 49-54.
Mosher HJ, Richardson KK, Lund BC: Sedative prescriptions are common at opioid initiation: An observational study in the veterans health administration. Pain Med. 2018; 19(4): 788-792.
Sun EC, Dixit A, Humphreys K, et al.: Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ. 2017; 356: j760.
Simon J, Gehret J, Stolzenberg D, et al.: Concomitant use of opioids and benzodiazepines in the outpatient setting. PM and R. 2019; 11(4): 337-343.
Gerlach LB, Olfson M, Kales HC, et al.: Opioids and other central nervous system-active polypharmacy in older adults in the United States. J Am Geriatr Soc. 2017; 65(9): 2052-2056.
Larochelle MR, Zhang F, Ross-Degnan D, et al.: Trends in opioid prescribing and co-prescribing of sedative hypnotics for acute and chronic musculoskeletal pain: 2001-2010. Pharmacoepidemiol Drug Saf. 2015; 24(8): 885-892.
Musich S, Wang SS, Slindee LB, et al.: Concurrent use of opioids with other central nervous system-active medications among older adults. Popul. Health Manag. 2019; 23: 286-296.
Cho J, Spence MM, Niu F, et al.: Risk of overdose with exposure to prescription opioids, benzodiazepines, and non-benzodiazepine sedative-hypnotics in adults: A retrospective cohort study. J Gen Intern Med. 2020; 35: 696-703.
Zhou L, Bhattacharjee S, Kwoh CK, et al.: Trends, patient and prescriber characteristics in gabapentinoid use in a sample of United States ambulatory care visits from 2003 to 2016. J Clin Med. 2019; 9(1): 83.
Payne RA: The epidemiology of polypharmacy. Clin Med. 2016; 16(5): 465.
Rasu R, Agbor-Bawa W, Rianon N: Impact of polypharmacy on seniors’ self-perceived health status. South Med J. 2017; 110(8): 540-545.
Rasu RS, Knell ME: Determinants of opioid prescribing for nonmalignant chronic pain in US outpatient settings. Pain Med. 2018; 19(3): 524-532.
Smith M, Giuliano MR, Starkowski MP: In Connecticut: Improving patient medication management in primary care. Health Aff. 2011; 30(4): 646-654.
Bingham JM, Taylor AM, Boesen KP, et al.: Preliminary investigation of pharmacist-delivered, direct-to-provider interventions to reduce co-prescribing of opioids and benzodiazepines among a medicare population. Pharmacy. 2020; 8(1): 25.
Tilli T, Hunchuck J, Dewhurst N, et al.: Opioid stewardship: Implementing a proactive, pharmacist-led intervention for patients coprescribed opioids and benzodiazepines at an urban academic primary care centre. BMJ Open Qual. 2020; 9(2): e000635.
Shehab N, Lovegrove MC, Geller AI, et al.: US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA. 2016; 316(20): 2115-2125.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.