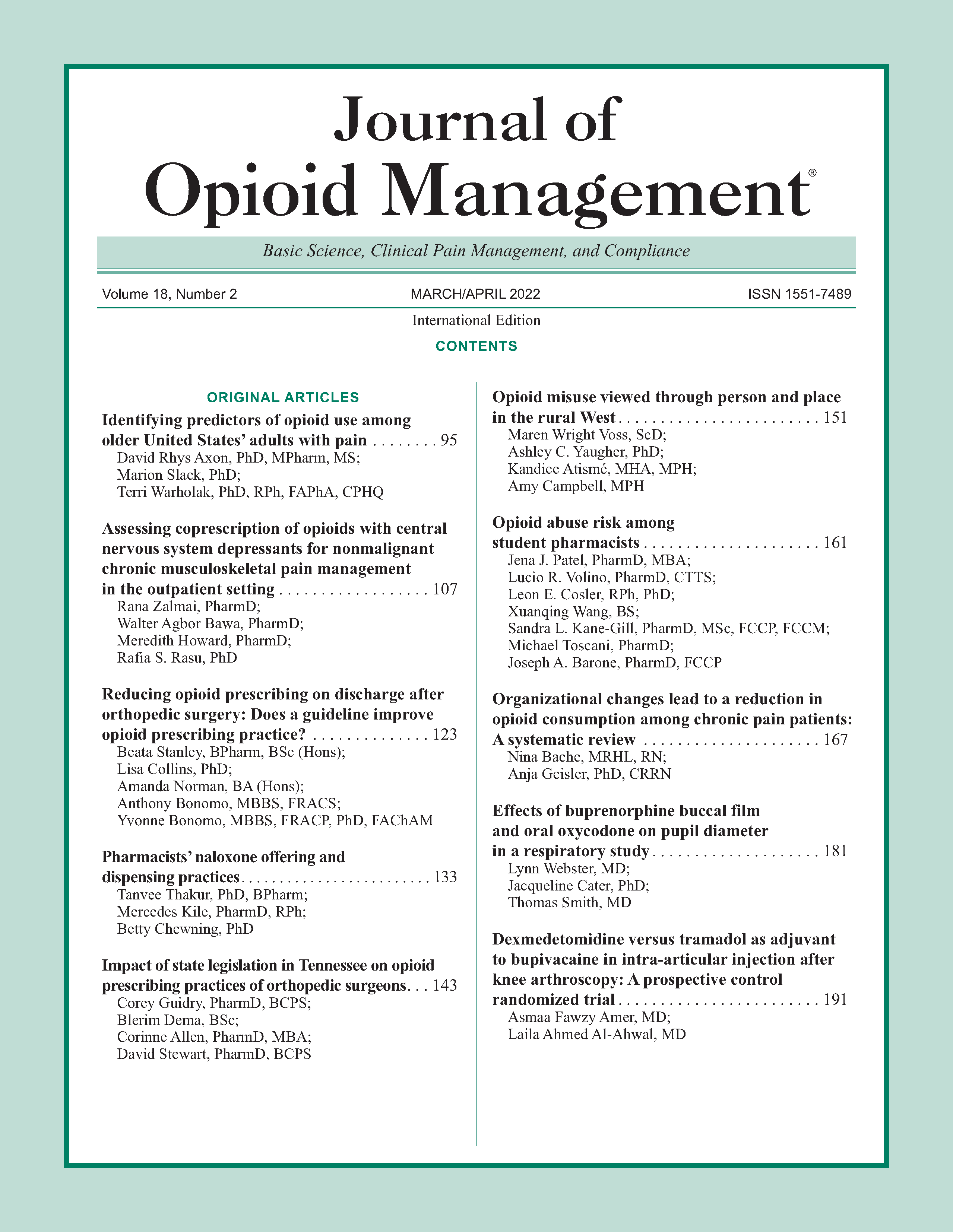
Opioid misuse viewed through person and place in the rural West
DOI:
https://doi.org/10.5055/jom.2022.0705Keywords:
rural, substance use, opioid, recovery, qualitativeAbstract
Objective: This article overviews the current statistics and factors related to increased rates of opioid use disorder (OUD) in rural areas, uncovering factors that may contribute to increased vulnerability to opioid overdose. We qualitatively review opinions, feelings, and thoughts surrounding this issue in rural areas of Utah, analyzing participant stories in reference to three themes through qualitative interviews, including the solitude of addiction, the beguiling strength of addiction, and one way out of addiction.
Design: In 2018, three focus groups were convened with 25 individuals from the rural area. Participants either currently or formerly (self-reported substance free for 6 months or more) experienced OUD with prescription opioids and heroin, or were family members of individuals who currently and formerly experienced OUD. These focus groups addressed current issues in OUDs in a rural Utah community related to person, place, and time. Following the focus groups, six individuals were invited to participate in semi-structured interviews. In-depth, semi-structured interviews queried individual experiences through a phenomenological approach, using a moderator guide with queries focused on identified themes related to the solitude, the intensity, and the difficulty escaping substance use disorder (SUD). Methodology included training community scholars with lived experience and member-checking to ensure phenomenological emphasis.
Results: Our qualitative reviews of the experience of OUD and SUD in rural Utah discussed the relevance and the nuance of the three identified themes. The interviewee statements further underscore the solitude, intensity, and difficulty of an individual's journey through SUD, the all-consuming nature of OUD, and the trouble that these factors cause in rural recovery.
Conclusions: We conclude that even during difficult situations in the rural experience with the opioid crisis, hope persists. OUD support in rurality may differ from the expected urban experience and include more coordination with criminal justice workers. Rural Americans have insights to share that could help turn the tide of this crisis.References
Hedegaard H, Warner M, Miniño, AM: Drug overdose deaths in the United States, 1999–2017. NCHS Data Brief, No. 329. Hyattsville, MD: National Center for Health Statistics. 2018, 2019.
Scholl L, Seth P, Kariisa M, et al.: Drug and opioid-involved overdose deaths—United States, 2013–2017. Morbidity Mortality Weekly Report. 2019; 67(5152): 1419.
Centers for Disease Control and Prevention. Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999—2008, 2011. Available at https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm. Accessed November 1, 2019.
Jones CM: Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers—United States, 2002–2004 and 2008–2010. Drug Alcohol Depen. 2013; 132(1-2): 95-100. DOI: 10.1016/j.drugalcdep.2013.01.007.
Hser YI, Mooney LJ, Saxon AJ, et al.: High mortality among patients with opioid use disorder in a large healthcare system. J Addict Med. 2017; 11(4): 315-319. DOI: 10.1097/adm.0000000000000312.
Monnat SM, Rigg KK: The opioid crisis in rural and small town America. Casey School of Public Policy Brief. 2018; 135.
Dahlhamer J, Lucas J, Zelaya C, et al.: Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018; 67(36): 1001-1006. DOI: 10.15585/mmwr.mm6736a2.
Prunuske JP, Hill CAS, Hager KD, et al.: Opioid prescribing patterns for non-malignant chronic pain for rural versus nonrural US adults: A population-based study using 2010 NAMCS data. BMC Health Serv Res. 2014; 14(1): 563.
Monnat SM, Rigg KK: Examining rural/urban differences in prescription opioid misuse among US adolescents. J Rural Health. 2016; 32(2): 204-218. DOI: 10.1111/jrh.12141.
Rigg KK, Monnat SM, Chavez MN: Opioid-related mortality in rural America: Geographic heterogeneity and intervention strategies. Int J Drug Policy. 2018; 57: 119-129.
Daniels ZM, VanLeit BJ, Skipper BJ: Factors in recruiting and retaining health professionals for rural practice. J Rural Health. 2007; 23(1): 62-71.
McCarty D, Priest KC, Korthuis PT, et al.: Treatment and prevention of opioid use disorder: Challenges and opportunities. Ann Rev Public Health. 2018; 39.
Sigmon SC: Access to treatment for opioid dependence in rural America: Challenges and future directions. JAMA Psychiatry. 2014; 71(4): 359-360. DOI: 10.1001/jamapsychiatry.2013.4450.
Pullen E, Oser C: Barriers to substance abuse treatment in rural and urban communities: counselor perspectives. Subst Use Misuse. 2014; 49(7): 891-901. DOI: 10.3109/10826084.2014.891615.
Dean SG, Hudson S, Hay-Smith EJC, et al.: Rural workers’ experience of low back pain: Exploring why they continue to work. J Occup Rehabil. 2011; 21(3): 395-409.
Keyes KM, Cerdá M, Brady JE, et al.: Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014; 104(2): e52-e59. DOI: 10.2105/AJPH.2013.301709.
Utah Department of Health: Prescription drug overdoses, 2017. Available at http://health.utah.gov/vipp/topics/prescription-drug-overdoses/ Accessed November 1, 2019.
Simoni JM, Weinberg BA, Nero DK: Training community members to conduct survey interviews: Notes from a study of seropositive women. AIDS Educ Prev. 1999; 11(1): 87.
Smythe EA, Pamela MI, Sims SL, et al.: Doing Heideggerian hermeneutic research: A discussion paper. Int J Nurs Stud. 2008; 45(9): 1389-1397. DOI: 10.1016/j.ijnurstu.2007.09.005.
Onwuegbuzie AJ, Dickinson WB, Leech NL, et al.: A qualitative framework for collecting and analyzing data in focus group research. Int J Qual Methods. 2009; 8(3): 1-21.
Reed KD, Hocking CS, Smythe LA, et al.: Exploring the meaning of occupation: the case for phenomenology. Can J Occup Ther. 2011; 78(5): 303-310. DOI: 10.2182/cjot.2011.78.5.5.
Gray JA, Hagemeier NE: Prescription drug abuse and DEA-sanctioned drug take-back events: characteristics and outcomes in rural Appalachia. Arch Int Med. 2012; 172(15): 1186-1187.
Yanovitzky I: The American medicine chest challenge: Evaluation of a drug take-back and disposal campaign. J Stud Alcohol Drugs. 2016; 77(4): 549-555.
Utah State Legislature: Budget deep dive into opioid outreach efforts (Legislative Financial Analyst), 2018. Available at https://le.utah.gov/interim/2017/pdf/00002833.pdf. Accessed March 9, 2021.
Kumpfer KL, Alvarado R, Whiteside HO: Family-based interventions for substance use and misuse prevention. Subst Use Misuse. 2003; 38(11-13): 1759-1787.
Modarai F, Mack K, Hicks P, et al.: Relationship of opioid prescription sales and overdoses, North Carolina. Drug and Alcohol Dependence, (2013, Sep 1). 132(1-2), 81-86. DOI: 10.1016/j.drugalcdep.2013.01.006.
Franklin GM, Mai J, Turner J, et al.: Bending the prescription opioid dosing and mortality curves: Impact of the Washington State opioid dosing guideline. Am J Ind Med. 2012; 55(4): 325-331.
Hoxmark E, Wynn TN: Loss of activities and its effect on the well-being of substance abusers. Scand J Occup Therapy. 2012; 19(1): 78-83.
Helbig K, McKay E: An exploration of addictive behaviours from an occupational perspective. J Occup Sci. 2003; 10(3): 140-145.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.