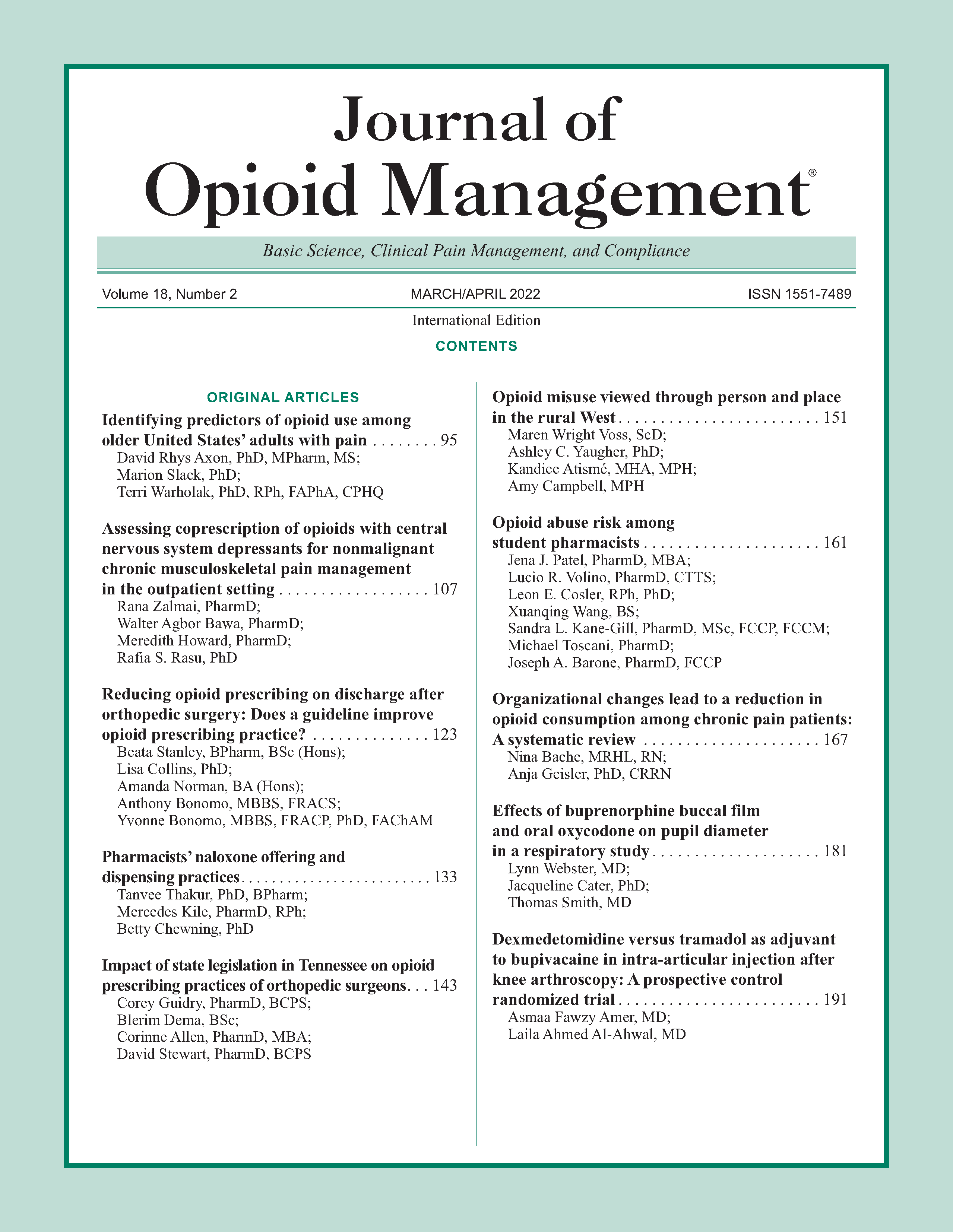
Effects of buprenorphine buccal film and oral oxycodone on pupil diameter in a respiratory study
DOI:
https://doi.org/10.5055/jom.2022.0708Keywords:
pupillometry, opioids, abuse, respiratory depressionAbstract
Objective: Evaluate the pupillary-constricting effects following administration of buprenorphine buccal film (BBF) and immediate-release (IR) oxycodone.
Design: A double-blind, double-dummy, six-treatment, six-period, placebo-controlled, randomized crossover study.
Setting: Single-center, phase 1 exploratory pharmacodynamics.
Participants: Healthy individuals who self-identify as recreational opioid users, confirmed via a naloxone challenge test on day 1.
Interventions: Placebo: BBF 300, 600, and 900 mcg and IR oxycodone 30 and 60 mg.
Main outcome measure: Minute ventilation (measured by the ventilator response to hypercapnia) and pupil diameter (determined via standard pupillometry) were assessed predose and at 0.5, 1, 1.5, 2, 2.5, 3, and 4 hours post-dose.
Results: Change from baseline in minute ventilation was moderately correlated with change from baseline in pupil diameter during treatment with BBF (Pearson's r = 0.38-0.40; p ≤ 0.0011) or oxycodone (Pearson's r = 0.34-0.37; p ≤ 0.005). The initial onset of significant (p < 0.05) pupil constriction relative to placebo occurred at 2, 1.5, and 1 hour after dosing with BBF 300, 600, and 900 mcg, respectively, and at 0.5 hours after dosing with oxycodone 30 or 60 mg.
Conclusions: Although BBF and IR oxycodone achieved similar levels of pupil constriction, there was a delayed miosis seen with BBF relative to that found with oxycodone.
References
Marshall B, Bland MK, Hulla R, et al.: Considerations in addressing the opioid epidemic and chronic pain within the USA. Pain Manag. 2019; 9(2): 131-138. DOI: 10.2217/pmt-2018-0070.
Dolinak D: Opioid toxicity. Acad Forensic Pathol. 2017; 7(1): 19-35. DOI: 10.23907/2017.003.
Pattinson KT: Opioids and the control of respiration. Br J Anaesth. 2008; 100(6): 747-758. DOI: 10.1093/bja/aen094.
Bauman V, Lopez I: Bloomberg Businessweek. Available at https://www.bloomberg.com/news/articles/2021-02-20/covidpandemic-has-only-made-the-opioid-crisis-worse. Accessed February 25, 2021.
Centers for Disease Control and Prevention: Overdose deaths accelerating during COVID-19. Available at https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html#:~:text=Over%2081%2C000%20drug%20overdose%20deaths,Control%20and%20Prevention%20(CDC). Accessed February 11, 2021.
Niles JK, Gudin J, Radcliff J, et al.: The opioid epidemic within the COVID-19 pandemic: Drug testing in 2020. Popul Health Manag. 2021; 24(S1): S43-S51. DOI: 10.1089/pop.2020.0230.
Larson MD, Behrends M: Portable infrared pupillometry: A review. Anesth Analg. 2015; 120(6): 1242-1253. DOI: 10.1213/ANE.0000000000000314.
Larson MD: Mechanism of opioid-induced pupillary effects. Clin Neurophysiol. 2008; 119(6): 1358-1364. DOI: 10.1016/j.clinph.2008.01.106.
Vaughan CW, Ingram SL, Connor MA, et al.: How opioids inhibit GABA-mediated neurotransmission. Nature. 1997; 390(6660): 611-614. DOI: 10.1038/37610.
Bachmutsky I, Wei XP, Kish E, et al. Opioids depress breathing through two small brainstem sites. Elife. 2020; 9. DOI: 10.7554/eLife.52694.
Le Merrer J, Becker JA, Befort K, et al.: Reward processing by the opioid system in the brain. Physiol Rev. 2009; 89(4): 1379-1412. DOI: 10.1152/physrev.00005.2009.
Mitsi V, Zachariou V: Modulation of pain, nociception, and analgesia by the brain reward center. Neuroscience. 2016; 338: 81-92. DOI: 10.1016/j.neuroscience.2016.05.017.
Kollars JP, Larson MD: Tolerance to miotic effects of opioids. Anesthesiology. 2005; 102(3): 701. DOI: 10.1097/00000542-200503000-00047.
Barvais L, Engelman E, Eba JM, et al.: Effect site concentrations of remifentanil and pupil response to noxious stimulation. Br J Anaesth. 2003; 91(3): 347-352. DOI: 10.1093/bja/aeg178.
Macleod DB, Habib AS, Ikeda K, et al.: Inhaled fentanyl aerosol in healthy volunteers: Pharmacokinetics and pharmacodynamics. Anesth Analg. 2012; 115(5): 1071-1077. DOI: 10.1213/ANE.0b013e3182691898.
Skarke C, Darimont J, Schmidt H, et al.: Analgesic effects of morphine and morphine-6-glucuronide in a transcutaneous electrical pain model in healthy volunteers. Clin Pharmacol Ther. 2003; 73(1): 107-121. DOI: 10.1067/mcp.2003.5.
Schoedel KA, McMorn S, Chakraborty B, et al.: Positive and negative subjective effects of extended-release oxymorphone versus controlled-release oxycodone in recreational opioid users. J Opioid Manag. 2011; 7(3): 179-192.
Walker DJ, Zacny JP: Subjective, psychomotor, and analgesic effects of oral codeine and morphine in healthy volunteers. Psychopharmacology (Berl). 1998; 140(2): 191-201. DOI: 10.1007/s002130050757.
Setnik B, Sommerville K, Goli V, et al.: Assessment of pharmacodynamics effects following oral administration of crushed morphine sulfate and naltrexone hydrochloride extended-release capsules compared with crushed morphine sulfate controlled-release tablets and placebo in nondependent recreational opioid users. Pain Med. 2013; 14(8): 1173-1186. DOI: 10.1111/pme.12148.
Webster LR, Johnson FK, Stauffer J, et al.: Impact of intravenous naltrexone on intravenous morphine-induced high, drug liking, and euphoric effects in experienced, nondependent male opioid users. Drugs R D. 2011; 11(3): 259-275. DOI: 10.2165/11593390-000000000-00000.
Kopecky EA, Fleming AB, Levy-Cooperman N, et al.: Oral human abuse potential of oxycodone DETERx® (Xtampza® ER). J Clin Pharmacol. 2017; 57(4): 500-512. DOI: 10.1002/jcph.833.
Shram MJ, Silverman B, Ehrich E, et al.: Use of remifentanil in a novel clinical paradigm to characterize onset and duration of opioid blockade by samidorphan, a potent mu-receptor antagonist. J Clin Psychopharmacol. 2015; 35(3): 242-249. DOI: 10.1097/JCP.0000000000000320.
Darwish M, Bond M, Ma Y, et al.: Abuse potential with oral route of administration of a hydrocodone extended-release tablet formulated with abuse-deterrence technology in nondependent, recreational opioid users. Pain Med. 2017; 18(1): 61-77. DOI: 10.1093/pm/pnw122.
Friedmann N, Marsman MR, de Kater AW, et al.: A nasal abuse potential randomized clinical trial of REMOXY(R) ER, a high-viscosity extended-release oxycodone formulation. J Opioid Manag. 2018; 14(6): 437-443.
Mickle TC, Guenther SM, Barrett AC, et al.: Pharmacokinetics and abuse potential of benzhydrocodone, a novel prodrug of hydrocodone, after intranasal administration in recreational drug users. Pain Med. 2018; 19(12): 2438-2449. DOI: 10.1093/pm/pnx247.
Morton TL, Devarakonda K, Kostenbader K, et al.: Correlation of subjective effects with systemic opioid exposure from fixed-dose combinations of oxycodone/acetaminophen in recreational users of prescription drugs. Pain Med. 2016; 17(3): 539-550.
Webster L, Henningfield J, Buchhalter AR, et al.: Human abuse potential of the new opioid analgesic molecule NKTR-181 compared with oxycodone. Pain Med. 2018; 19(2): 307-318. DOI: 10.1093/pm/pnw344.
Webster LR, Kopecky EA, Smith MD, et al.: A randomized, double-blind, double-dummy study to evaluate the intranasal human abuse potential and pharmacokinetics of a novel extended-release abuse-deterrent formulation of oxycodone. Pain Med. 2016; 17(6): 1112-1130.
Webster LR, Rolleri RL, Pixton GC, et al.: Randomized, double-blind, placebo-controlled and active-controlled study to assess the relative abuse potential of oxycodone HCl-niacin tablets compared with oxycodone alone in nondependent, recreational opioid users. Subst Abuse Rehabil. 2012; 3: 101-113. DOI: 10.2147/SAR.S33080.
Webster LR, Smith MD, Lawler J, et al.: Human abuse potential of an abuse-deterrent (AD), extended-release (ER) morphine product candidate (morphine-ADER injection-molded tablets) vs extended-release morphine administered intranasally in nondependent recreational opioid users. Pain Med. 2017; 18(9): 1695-1705.
Rollins MD, Feiner JR, Lee JM, et al.: Pupillary effects of high-dose opioid quantified with infrared pupillometry. Anesthesiology. 2014; 121(5): 1037-1044. DOI: 10.1097/ALN.0000000000000384.
Dahan A, Yassen A, Bijl H, et al.: Comparison of the respiratory effects of intravenous buprenorphine and fentanyl in humans and rats. Br J Anaesth. 2005; 94(6): 825-834. DOI: 10.1093/bja/aei145.
Dahan A, Yassen A, Romberg R, et al.: Buprenorphine induces ceiling in respiratory depression but not in analgesia. Br J Anaesth. 2006; 96(5): 627-632. DOI: 10.1093/bja/ael051.
Webster LR, Hansen E, Cater J, et al.: A phase I placebo-controlled trial comparing the effects of buprenorphine buccal film and oral oxycodone hydrochloride administration on respiratory drive. Adv Ther. 2020; 37(11): 4685-4696. DOI: 10.1007/s12325-020-01481-0.
Rauck RL, Potts J, Xiang Q, et al.: Efficacy and tolerability of buccal buprenorphine in opioid-naive patients with moderate to severe chronic low back pain. Postgrad Med. 2016; 128(1): 1-11. DOI: 10.1080/00325481.2016.1128307.
Gimbel J, Spierings ELH, Katz N, et al.: Efficacy and tolerability of buccal buprenorphine in opioid-experienced patients with moderate to severe chronic low back pain: Results of a phase 3, enriched enrollment, randomized withdrawal study. Pain. 2016; 157(11): 2517-2526. DOI: 10.1097/j.pain.0000000000000670.
Jasinski DR, Pevnick JS, Griffith JD: Human pharmacology and abuse potential of the analgesic buprenorphine: A potential agent for treating narcotic addiction. Arch Gen Psychiatry. 1978; 35(4): 501-516. DOI: 10.1001/archpsyc.1978.01770280111012.
Yokell MA, Zaller ND, Green TC, et al.: Buprenorphine and buprenorphine/naloxone diversion, misuse, and illicit use: An international review. Curr Drug Abuse Rev. 2011; 4(1): 28-41.
Belbuca [package insert]. Raleigh, NC: BioDelivery Sciences International Inc., 2019.
United States Drug Enforcement Administration: Drug scheduling. Available at https://www.dea.gov/drug-scheduling. Accessed December 15, 2020.
Zamani N, Buckley NA, Hassanian-Moghaddam H: Buprenorphine to reverse respiratory depression from methadone overdose in opioid-dependent patients: A prospective randomized trial. Crit Care. 2020; 24(1): 44. DOI: 10.1186/s13054-020-2740-y.
Khanna IK, Pillarisetti S: Buprenorphine—An attractive opioid with underutilized potential in treatment of chronic pain. J Pain Res. 2015; 8: 859-870.
Rorick-Kehn LM, Witcher JW, Lowe SL, et al.: Determining pharmacological selectivity of the kappa opioid receptor antagonist LY2456302 using pupillometry as a translational biomarker in rat and human. Int J Neuropsychopharmacol. 2014; 18(2): pyu036.
McAnany JJ, Smith BM, Garland A, et al.: iPhone-based pupillometry: A novel approach for assessing the pupillary light reflex. Optom Vis Sci. 2018; 95(10): 953-958. DOI: 10.1097/OPX.0000000000001289.
Downloads
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.