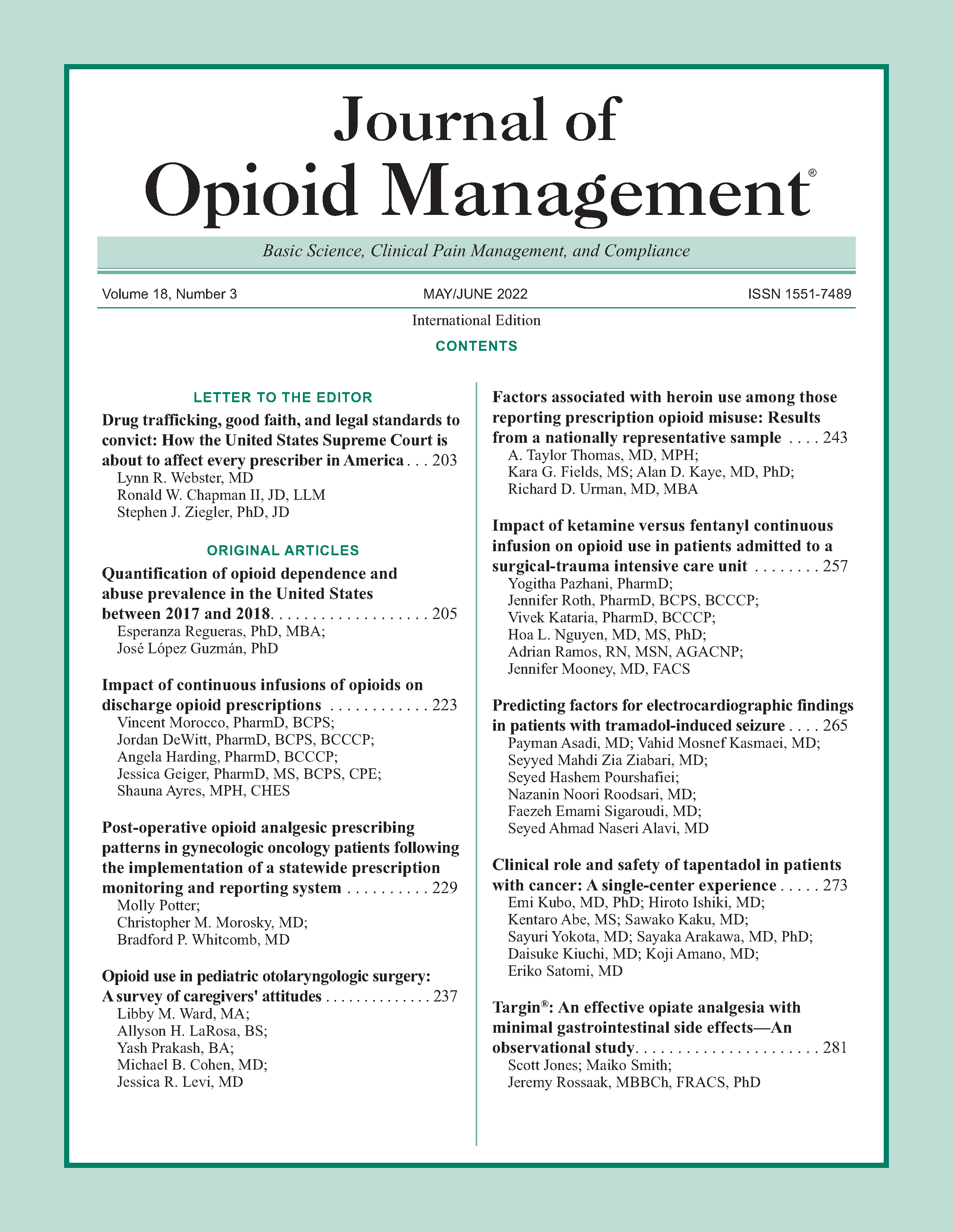
Impact of continuous infusions of opioids on discharge opioid prescriptions
DOI:
https://doi.org/10.5055/jom.2022.0713Keywords:
critical care, opioid, mechanical ventilation, analgesia, sedation, analagosedation, opioid epidemic, painAbstract
Introduction: The 2018 Pain, Agitation/Sedation, Delirium, Immobility, and Sleep guidelines from the Society of Critical Care Medicine recommend opioids as a first-line treatment option for non-neuropathic pain among critically ill adults and prioritize pain management optimization before the administration of sedatives. Although analagosedation is recommended, the downstream effects, such as intensive care unit (ICU)-acquired opioid dependence, are not well described. The purpose of this study is to determine the impact of continuous infusions of opioids for mechanically ventilated patients prescribed opioids on discharge.
Methods: This was a single-center, retrospective chart review of mechanically ventilated patients admitted to the medical ICU at a tertiary medical center from July 1, 2018 to June 30, 2019. The primary objective of this study was to compare the incidence of opioid prescriptions at discharge between those who received opioid infusions versus intermittent administrations. Secondary objectives included risk factors for receiving opioid prescriptions at discharge and readmission within 90 days with an active opioid prescription and/or a diagnosis of opioid use disorder.
Results: A total of 100 patients were included. There was no statistically significant difference in the incidence of opioid prescriptions at discharge between the groups (p = 0.933). Only one patient was readmitted within 90 days with documented opioid use disorder and 11 patients with prescription opioids on their home medication list. A best-fit logistic regression model including the type of opioid administration (p = 0.275), length of stay (p = 0.018), and opioid dose (p = 0.137) showed that length of stay was the only significant predictor of discharge opioid prescribing.
Conclusion: The incidence of opioid prescriptions at discharge for critically ill, mechanically ventilated patients did not differ based on opioid administration strategy. ICU length of stay appears to be a predictive factor of opioid discharge prescriptions.
References
Kram B, Weigel K, Kuhrt M, et al.: Discharge prescribing of enteral opioids after initiation as a weaning strategy from continuous opioid infusions in the intensive care unit. J Opioid Manag. 2018; 14(1): 35.
Devlin J, Skrobik Y, Gélinas C, et al.: Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018; 46(9): e825-e873.
Cammarano W, Pittet J-F, Weitz S, et al.: Acute withdrawal syndrome related to the administration of analgesic and sedative medications in adult intensive care unit patients. Crit Care Med. 1998; 26(4): 676-684.
Jacobi J, Fraser GL, Coursin DB, et al.: Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. AJHP. 2002; 59(2): 150-178.
Puntillo K, Naidu R: Chronic pain disorders after critical illness and ICU-acquired opioid dependence: Two clinical conundra. Curr Opin Crit Care. 2016; 22(5): 506-512.
Morandi A, Vasilevskis E, Pandharipande P, et al.: Inappropriate medication prescriptions in elderly adults surviving an intensive care unit hospitalization. J Am Geriatr Soc. 2013; 61(7): 1128-1134.
Kirton O: Mechanical ventilation in the intensive care unit. The American Association for the Surgery of Trauma. Available at https://www.aast.org/GeneralInformation/mechanicalventilation.aspx. Accessed May 1, 2020.
Wilson N: Drug and opioid-involved overdose deaths—United States, 2017. MMWR Morb Mortal Wkly Rep. 2020; 69(11): 290-297.
CDC Wonder: Online database. Available at https://wonder.cdc.gov/. Accessed May 1, 2020.
Bedene A, Lijfering WM, Niesters M, et al.: Opioid prescription patterns and risk factors associated with opioid use in The Netherlands. JAMA Netw Open. 2019; 2(8): e1910223. DOI: 10.1001/jamanetworkopen.2019.10223.
Tully A, Hammond D, Li C, et al.: Evaluation of medication errors at the transition of care from an ICU to non-ICU location. Crit Care Med. 2019; 47(4): 543-549.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.