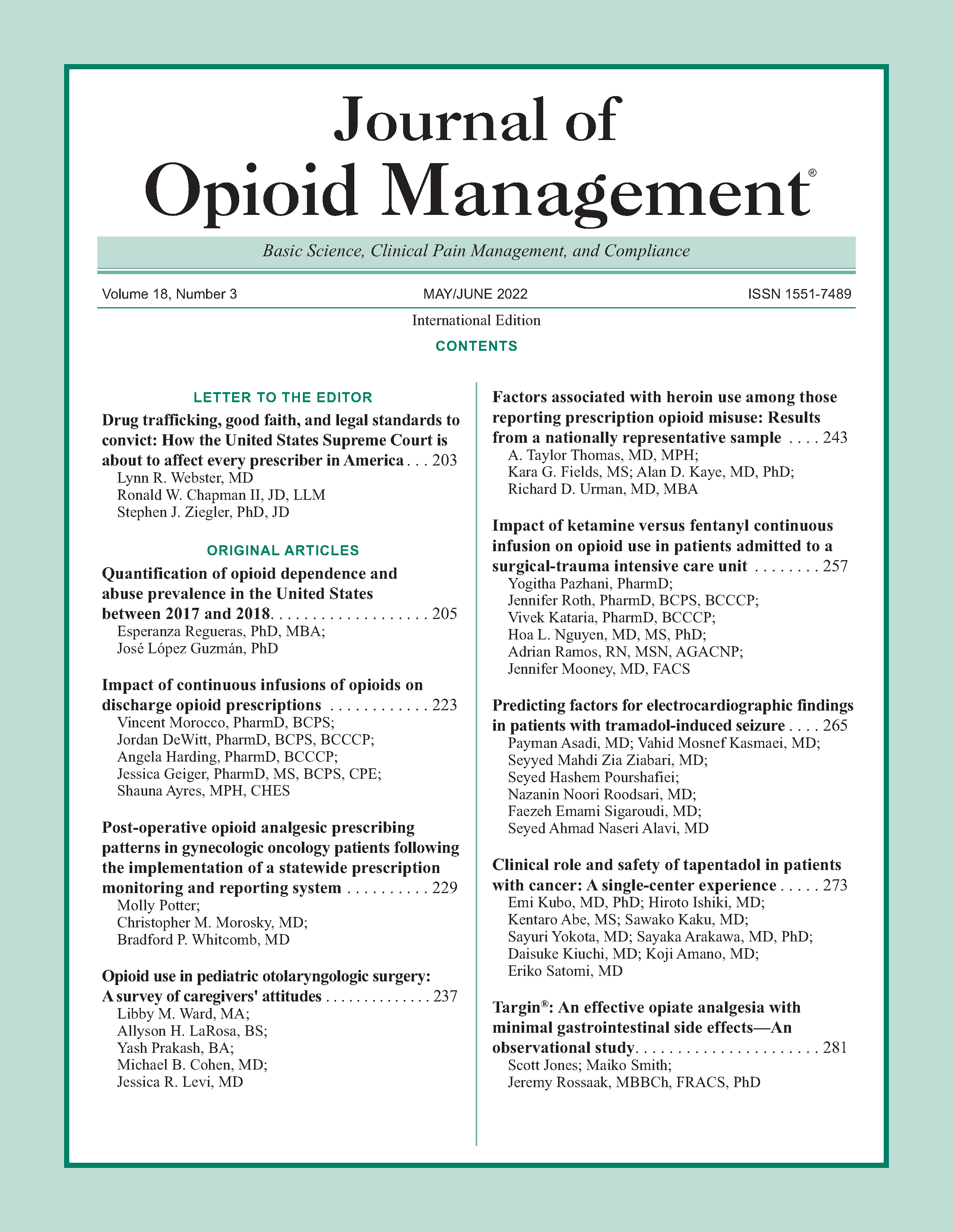
Factors associated with heroin use among those reporting prescription opioid misuse: Results from a nationally representative sample
DOI:
https://doi.org/10.5055/jom.2022.0716Keywords:
heroin, opioid, drug abuse, substance abuse, opioid epidemicAbstract
Objective: The present investigation aims to identify characteristics associated with heroin use among those reporting prescription opioid misuse from a nationally representative sample, and how these characteristics vary by urbanicity.
Design: A cross-sectional analysis.
Setting: Pooled 2015-2018 data from the National Survey on Drug Use and Health (NSDUH), the leading source for nationally representative substance use, mental health, and other health-related data and trends in the United States.
Patients and participants: 23,719 participants (12,109 male and 11,610 female) reporting previous prescription opioid misuse in the 2015-2018 NSDUH data.
Interventions: None.
Main outcome measures: Univariable and multivariable logistic regressions were used to assess the association of characteristics with heroin use, stratified by urbanicity.
Results: After multivariable adjustment, factors associated with heroin use among prescription opioid misusers were male sex, non-Hispanic White race, low educational attainment, recent nonopioid illicit drug use, and recent nonopioid prescription drug misuse. Commercial health insurance was associated with lower odds of heroin use among both rural and urban prescription opioid misusers, but an observed association between Medicaid and greater odds of heroin use was stronger among urban versus rural participants. In contrast, observed associations between illicit drug use other than marijuana in the past year and greater odds of heroin use were stronger among rural vs urban participants.
Conclusion: Important differences exist between factors associated with heroin use among urban and rural prescription opioid misusers, and there is a need to consider broader polysubstance use trends and barriers to mental healthcare access to adequately address heroin use.
References
Grau LE, Dasgupta N, Harvey AP, et al.: Illicit use of opioids: Is OxyContin a “gateway drug”? Am J Addict. 2007; 16(3): 166-173. DOI: 10.1080/10550490701375293.
Kanouse AB, Compton P: The epidemic of prescription opioid abuse, the subsequent rising prevalence of heroin use, and the federal response. J Pain Palliat Care Pharmacother. 2015; 29(2): 102-114. DOI: 10.3109/15360288.2015.1037521.
Cicero TJ, Ellis MS, Surratt HL, et al.: The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry. 2014; 71(7): 821-826. DOI: 10.1001/jamapsychiatry.2014.366.
Lankenau SE, Teti M, Silva K, et al.: Initiation into prescription opioid misuse amongst young injection drug users. Int J Drug Policy. 2012; 23(1): 37-44. DOI: 10.1016/j.drugpo.2011.05.014.
Jones CM, Logan J, Gladden M, et al.: Vital signs: Demographic and substance use trends among heroin users—United States, 2002–2013. 2015: 719-725. Available at https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6426a3.htm. Accessed November 15, 2021.
Muhuri PK, Gfroerer JC, Davies MC: Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Rev. 2013. Available at https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-painreliever-use-2013.htm. Accessed November 15, 2021.
Mars SG, Ondocsin J, Ciccarone D: Sold as heroin: Perceptions and use of an evolving drug in Baltimore, MD. J Psychoactive Drugs. 2018; 50(2): 167-176. DOI: 10.1080/02791072.2017.1394508.
Compton WM, Jones CM, Baldwin GT: Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016; 374(2): 154-163.
Rigg KK, Monnat SM: Urban vs. rural differences in prescription opioid misuse among adults in the United States: Informing region specific drug policies and interventions. Int J Drug Policy. 2015; 26(5): 484-491. DOI: 10.1016/j.drugpo.2014.10.001
US Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2015 (NSDUH-2015-DS0001). 2018. Available at https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health. Accessed November 15, 2021.
US Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2016 (NSDUH-2016-DS0001. 2018. Available at https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2018R2/NSDUHDetailedTabs2018.pdf. Accessed November 15, 2021.
US Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2017 (NSDUH-2017-DS0001). 2018. Available at https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf. Accessed November 15, 2021.
US Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality: National Survey on Drug Use and Health 2018 (NSDUH-2018-DS0001). 2019. Available at https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHMethodsSummDefs2018/NSDUHMethodsSummDefs2018.htm. Accessed November 15, 2021.
CDC: Annual surveillance report of drug-related risks and outcomes—United States surveillance special report. Atlanta, Georgia: Centers for Disease Control and Prevention, US Department of Health and Human Services, 2019.
Center for Behavioral Health Statistics and Quality: 2016 national survey on drug use and health public use file codebook. 2018. Available at https://www.samhsa.gov/data/. Accessed November 15, 2021.
Substance Abuse and Mental Health Services Administration: Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. 2019. Available at https://www.samhsa.gov/data/. Accessed November 15, 2021.
Havens JR, Young AM, Havens CE: Nonmedical prescription drug use in a nationally representative sample of adolescents: Evidence of greater use among rural adolescents. Arch Pediatr Adolesc Med. 2011; 165(3): 250-255. DOI: 10.1001/archpediatrics.2010.217.
Mital S, Windle M, Cooper HLF, et al.: Trends in non-medical prescription opioids and heroin co-use among adults, 2003-2014. Addict Behav. 2018; 86: 17-23. DOI: 10.1016/j.addbeh.2018.05.005.
Pear VA, Ponicki WR, Gaidus A, et al.: Urban-rural variation in the socioeconomic determinants of opioid overdose. Drug Alcohol Depend. 2019; 195: 66-73. DOI: 10.1016/j.drugalcdep.2018.11.024.
Smart RG: An availability-proneness theory of illicit drug abuse. NIDA Res Monogr. 1980; 30: 46-49.
Rigg KK, Murphy JW: Understanding the etiology of prescription opioid abuse: Implications for prevention and treatment. Qual Health Res. 2013; 23(7): 963-975. DOI: 10.1177/1049732313488837.
Jones DS: How personalized medicine became genetic, and racial: Werner Kalow and the formations of pharmacogenetics. J History Med Allied Sci. 2013; 68(1): 1-48. DOI: 10.1093/jhmas/jrr046.
Pullen E, Oser C: Barriers to substance abuse treatment in rural and urban communities: A counselor perspective. Subst Use Misuse. 2014; 49(7): 891-901. DOI: 10.3109/10826084.2014.891615.
Keyes KM, Cerdá M, Brady JE, et al.: Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. Am J Public Health. 2014; 104(2): e52-e59. DOI: 10.2105/AJPH.2013.301709.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.