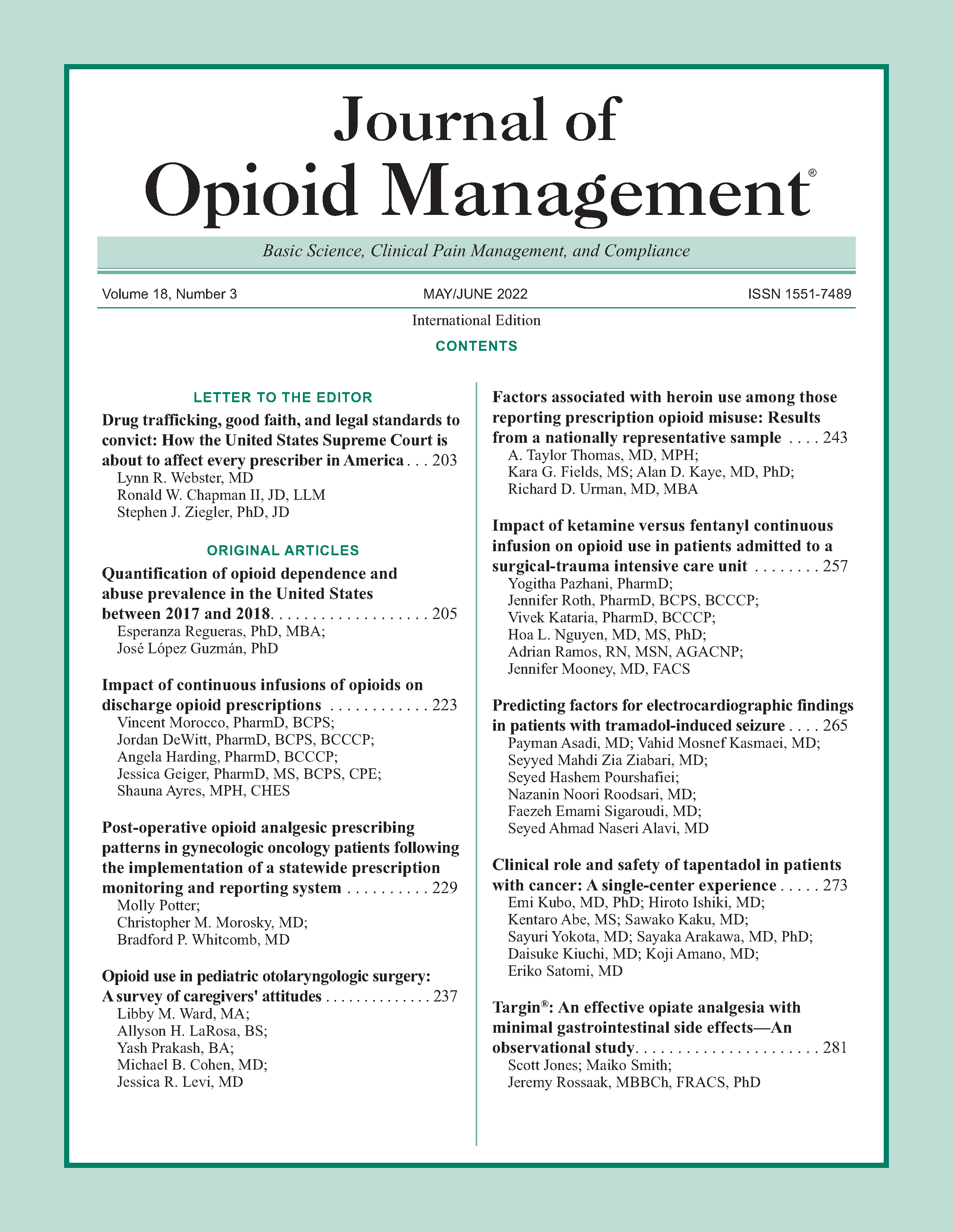
Impact of ketamine versus fentanyl continuous infusion on opioid use in patients admitted to a surgical-trauma intensive care unit
DOI:
https://doi.org/10.5055/jom.2022.0717Keywords:
ketamine, fentanyl, analgesia management, trauma, surgeryAbstract
Objective: Ketamine has been shown to decrease opioid utilization as an adjunct, but limited evidence is available on ketamine as a primary analgesic strategy.
Design: A retrospective chart review.
Patients and participants: Mechanically ventilated adult patients (≥18 years) in the surgery-trauma intensive care unit (STICU) with continuous infusion ketamine or fentanyl with concomitant propofol for at least 12 hours were screened for inclusion. The final analysis included 22 patients in the ketamine/propofol (KP) group and 24 patients in the fentanyl/propofol (FP) group.
Interventions: Patients in the STICU received KP or FP continuous infusions.
Main outcome measures: The primary outcome compared opioid requirements between both groups during mechanical ventilation.
Results: The median opioid requirement during mechanical ventilation was significantly higher in the FP group compared to the KP group (median 1,392 milligrams of morphine equivalents (MMEs) [interquartile range (IQR) 709.5-2,292] versus 206.3 MME [IQR 87-510], p < 0.001). After extubation, there was no difference in opioid utilization. Patients in the KP group spent less time at goal Critical Care Pain Observation Tool compared to the FP group (median 77.6 percent, IQR [71.9-85.2] versus 88.9 percent, IQR [76.9-97.4], p = 0.003). The proportions of patients developing adverse effects were not significantly different between the two groups.
Conclusions: Among critically ill mechanically ventilated patients in the STICU, continuous ketamine resulted in significantly less opioids during mechanical ventilation. Further studies with a larger sample size are needed to assess the appropriate dosing strategy for ketamine to produce adequate analgesia when used as a primary analgesic in mechanically ventilated patients.
References
Garber PM, Droege CA, Carter KE, et al.: Continuous infusion ketamine for adjunctive analgosedation in mechanically ventilated, critically ill patients. Pharmacotherapy. 2019; 39(3): 288-296.
Hamrick KL, Beyer CA, Lee JA, et al.: Multimodal analgesia and opioid use in critically ill trauma patients. J Am Coll Surg. 2019; 228(5): 769-775.
Devlin JW, Skrobik Y, Gelinas C, et al.: Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018; 46(9): e825-e873.
Pruskowski KA, Harbourt K, Pajoumand M, et al.: Impact of ketamine use on adjunctive analgesic and sedative medications in critically ill trauma patients. Pharmacotherapy. 2017; 37(12): 1537-1544.
Shurtleff V, Radosevich JJ, Patanwala AE: Comparison of ketamine-versus nonketamine-based sedation on delirium and coma in the intensive care unit. J Intensive Care Med. 2020; 35(6): 536-541.
Manasco AT, Stephens RJ, Yaeger LH, et al.: Ketamine sedation in mechanically ventilated patients: A systematic review and meta-analysis. J Crit Care. 2020; 56: 80-88.
Buchheit JL, Yeh DD, Eikermann M, et al.: Impact of low-dose ketamine on the usage of continuous opioid infusion for the treatment of pain in adult mechanically ventilated patients in surgical intensive care units. J Intensive Care Med. 2019; 34(8): 646-651.
Groetzinger LM, Rivosecchi RM, Bain W, et al.: Ketamine infusion for adjunct sedation in mechanically ventilated adults. Pharmacotherapy. 2018; 38(2): 181-188.
Visser E, Schug SA: The role of ketamine in pain management. Biomed Pharmacother. 2006; 60(7): 341-348.
Hurth KP, Thomas KB, Rudoni MA, et al.: The reemergence of ketamine for treatment in critically ill adults. Crit Care Med. 2020; 48(6): 899-911.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain. 2016; 65(No. RR-1): 1-49.
Knotkova H, Fine PG, Portenoy RK: Opioid rotation: The science and the limitations of equianalgesic dose table. J Pain Symptom Manage. 2009; 38(3): 426-439.
Choi L, Ferrell BA, Vasilevskis EE, et al.: Population pharmacokinetics of fentanyl in the critically ill. Crit Care Med. 2016; 44(1): 64-72.
Severgnini P, Pelosi P, Contino E, et al.: Accuracy of critical care pain observation tool and behavioral pain scale to assess pain in critically ill conscious and unconscious patients: Prospective, observational study. J Intensive Care. 2016; 4(68): 1-8.
Patanwala AE, Aljuhani O, Kopp BJ, et al.: Methocarbamol use is associated with decreased hospital length of stay in trauma patients with closed rib fractures. Am J Surg. 2017; 214(4): 738-742.
Aljuhani O, Kopp BJ, Patanwala AE: Effect of methocarbamol on acute pain after traumatic injury. Am J Ther. 2017; 24(2): e202-e206.
Ingrande J, Lemmens HJM: Dose adjustments of anaesthetics in the morbidly obese. Br J Anaesth. 2010; 105(Suppl. 1): i16-i23. DOI: 10.1093/bja/aeq312
Wulfsohn NL: Ketamine dosage for induction based on lean body mass. Anesth Analg. 1972; 51(2): 299-305.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.