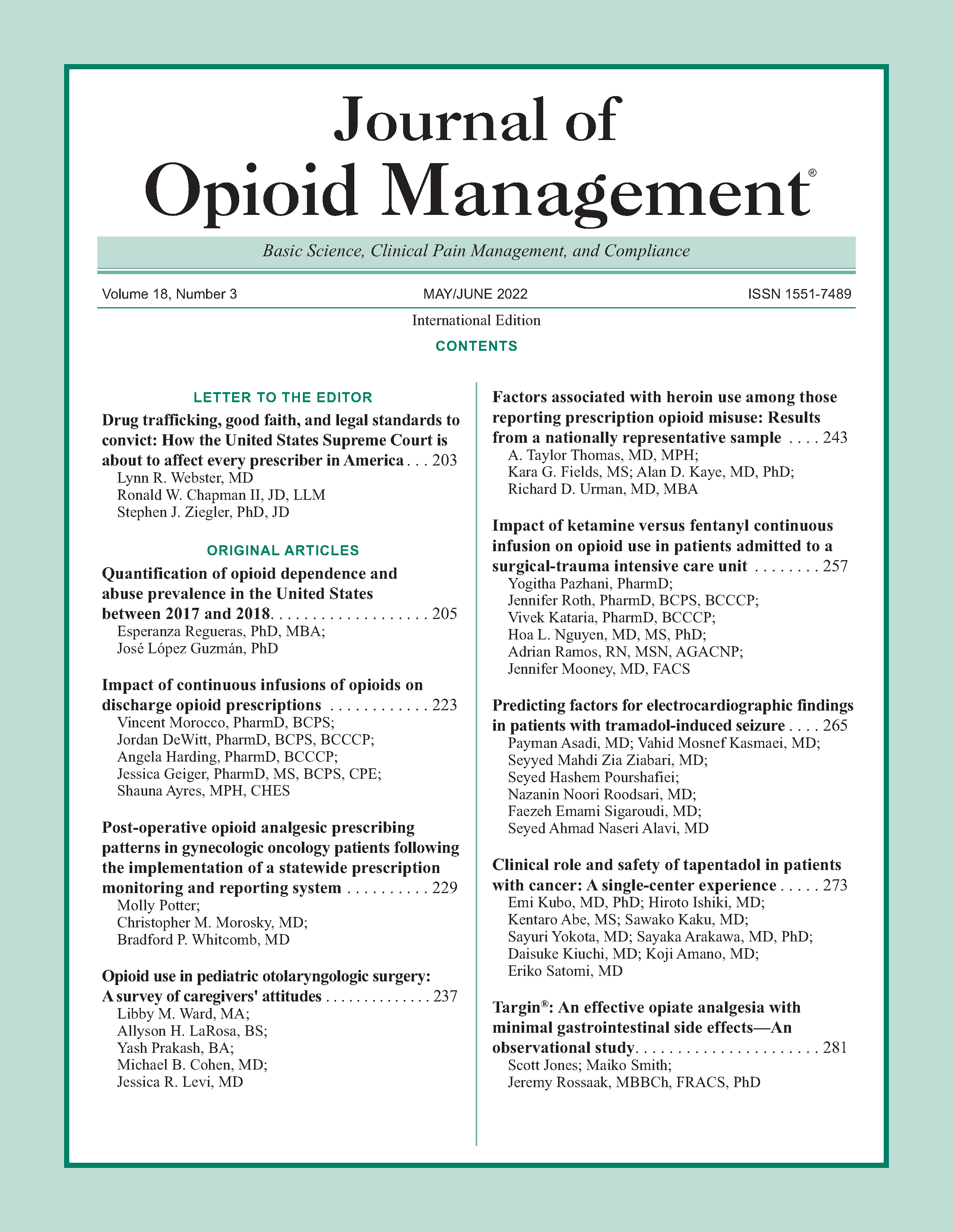
Targin®: An effective opiate analgesia with minimal gastrointestinal side effects—An observational study
DOI:
https://doi.org/10.5055/jom.2022.0721Keywords:
oxycodone, naloxone, post-operative ileusAbstract
Objective: To examine the role of Targin® (oral oxycodone:naloxone combination) in the perioperative setting.
Design: A single center prospective observational pilot study at a regional hospital.
Setting: Thirty-eight eligible patients undergoing major general surgical operations were recruited. Thirty-two patients completed the study.
Interventions: Participants were given Targin twice daily from day 2 postoperatively with twice daily measures of pain scores, gut function, and mobility.
Main outcome measures: The primary end points were analgesic efficacy and the rate of ileus. Secondary end points were gastrointestinal (GI) recovery and the need for opioid requirement on discharge, at 1 week and 1 month.
Results: Average pain score over 5 days at rest was one and on movement was four out of 10. All patients mobilized to a chair by day 3. Twenty-six participants (81.3 percent) experienced nausea at some point during the study, and four participants (12.5 percent) were diagnosed with a post-operative ileus (POI). There was no serious adverse event reported. Only two patients were on opioids at 1-month discharge. This was due to them having Orthopaedic surgery not related to this study.
Conclusions: Targin appears to provide effective analgesia when used responsibly in elective post-operative GI surgical patients, with a low rate of POI and long-term opiate use.
References
Asgeirsson T, El-Badawi KI, Mahmood A, et al.: Postoperative ileus: It costs more than you expect. J Am Coll Surg. 2010; 210(2): 228-231.
Augestad KM, Delaney CP: Postoperative ileus: Impact of pharmacological treatment, laparoscopic surgery and enhanced recovery pathways. World J Gastroenterol. 2010; 16(17): 2067-2074.
Vather R, Trivedi S, Bissett I: Defining postoperative ileus: Results of a systematic review and global survey. J Gastrointest Surg. 2013; 17(5): 962-972.
Kehlet H, Holte K: Review of postoperative ileus. Am J Surg. 2001; 182: S3-S10.
Beard TL, Leslie JB, Nemeth J: The opioid component of delayed gastrointestinal recovery after bowel resection. J Gastrointest Surg. 2011; 15(7): 1259-1268.
Vather R, O’Grady G, Bissett IP, et al.: Postoperative ileus: Mechanisms and future directions for research. Clin Exp Pharmacol Physiol. 2014; 41(5): 358-370.
Kuusniemi K, Zollner J, Sjövall S, et al.: Prolonged-release oxycodone/naloxone in postoperative pain management: From a randomized clinical trial to usual clinical practice. J Int Med Res. 2012; 40(5): 1775-1793.
Ho HS: Patient-controlled analgesia versus oral controlled-release oxycodone—Are they interchangeable for acute postoperative pain after laparoscopic colorectal surgeries? Oncology. 2008; 74(1): 61-65.
Miedema BW, Johnson JO: Methods for decreasing post-operative gut dysmotility. Lancet Oncol. 2003; 4(6): 365-372.
Holzer P: Opioid receptors in the gastrointestinal tract. Regul Pept. 2009; 155(1): 11-17.
DeSchepper HU, Cremonini F, Park MI, et al.: Opioids and the gut: Pharmacology and current clinical experience. Neurogastroenterol Motil. 2004; 16(4): 383-394.
Scott MJ, McEvoy MD, Gordon DB, et al.: American society for enhanced recovery (ASER) and perioperative quality initiative (POQI) joint consensus statement on optimal analgesia within an enhanced recovery pathway for colorectal surgery: Part 2—from PACU to the transition home. Perioper Med. 2017; 6: 7.
Hakkarainen TW, Steele SR, Bastaworous A, et al.: Nonsteroidal anti-inflammatory drugs and the risk for anastomotic failure. JAMA Surg. 2015; 150(3): 223.
Schutter U, Grunert S, Meyer C, et al.: Innovative pain therapy with a fixed combination of prolonged-release oxycodone/naloxone: A large observational study under conditions of daily practice. Curr Med Res Opin. 2010; 26(6): 1377-1387.
Pardo MC, Miler RD (eds.): Opioids (Chapter 9). In Basics of Anesthesia, 7th ed. Philadelphia: Elsevier, 2017: 123-138.
Smith K, Hopp M, Mundin G, et al.: Naloxone as part of a prolonged release oxycodone/naloxone combination reduces oxycodone-induced slowing of gastrointestinal transit in healthy volunteers. Expert Opin Invest Drugs. 2011; 20(4): 427-439.
Burness CB, Keating GM: Oxycodone/naloxone prolonged-release: A review of its use in the management of chronic pain while counteracting opioid-induced constipation. Drugs. 2014; 74(3): 353-375.
Simpson K, Leyendecker P, Hopp M, et al.: Fixed-ratio combination oxycodone/naloxone compared with oxycodone alone for the relief of opioid-induced constipation in moderate-to-severe noncancer pain. Curr Med Res Opin. 2008; 24(12): 3503-3512.
Ahmedzai SH, Nauck F, Bar-Sela G, et al.: A randomized, double-blind, active-controlled, double-dummy, parallel-group study to determine the safety and efficacy of oxycodone/naloxone prolonged-release tablets in patients with moderate/severe, chronic cancer pain. Palliat Med. 2012; 26(1): 50-60.
Meissner W, Leyendecker P, Mueller-Lissner S, et al.: A randomized controlled trial with prolonged-release oral oxycodone and naloxone to prevent and reverse opioid-induced constipation. 2009; 13(1): 56-64.
Millan M, Biondo S, Cracklier D, et al.: Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J Surg. 2012; 36(1): 179-185.
Delaney CP, Weese JL, Hyman NH, et al.: Phase III trial of alvimopan, a novel, peripherally acting, mu opioid antagonist, for postoperative ileus after major abdominal surgery. Dis Colon Rectum. 2005; 48(6): 1114-1129.
Comelon M, Wisloeff-Aase K, Raeder J, et al.: A comparison of oxycodone prolonged-release vs. oxycodone + naloxone prolonged-release after laparoscopic hysterectomy. Acta Anaesthesiol Scand. 2013; 57(4): 509-517.
Creamer F, Balfour A, Nimmo S, et al.: Randomized open-label phase II study comparing oxycodone-naloxone with oxycodone in early return of gastrointestinal function after laparoscopic colorectal surgery. Br J Surg. 2016; 104(1): 42-51.
Leon C, Davis L, Kraemer H: The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011; 45(5): 626-629.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.