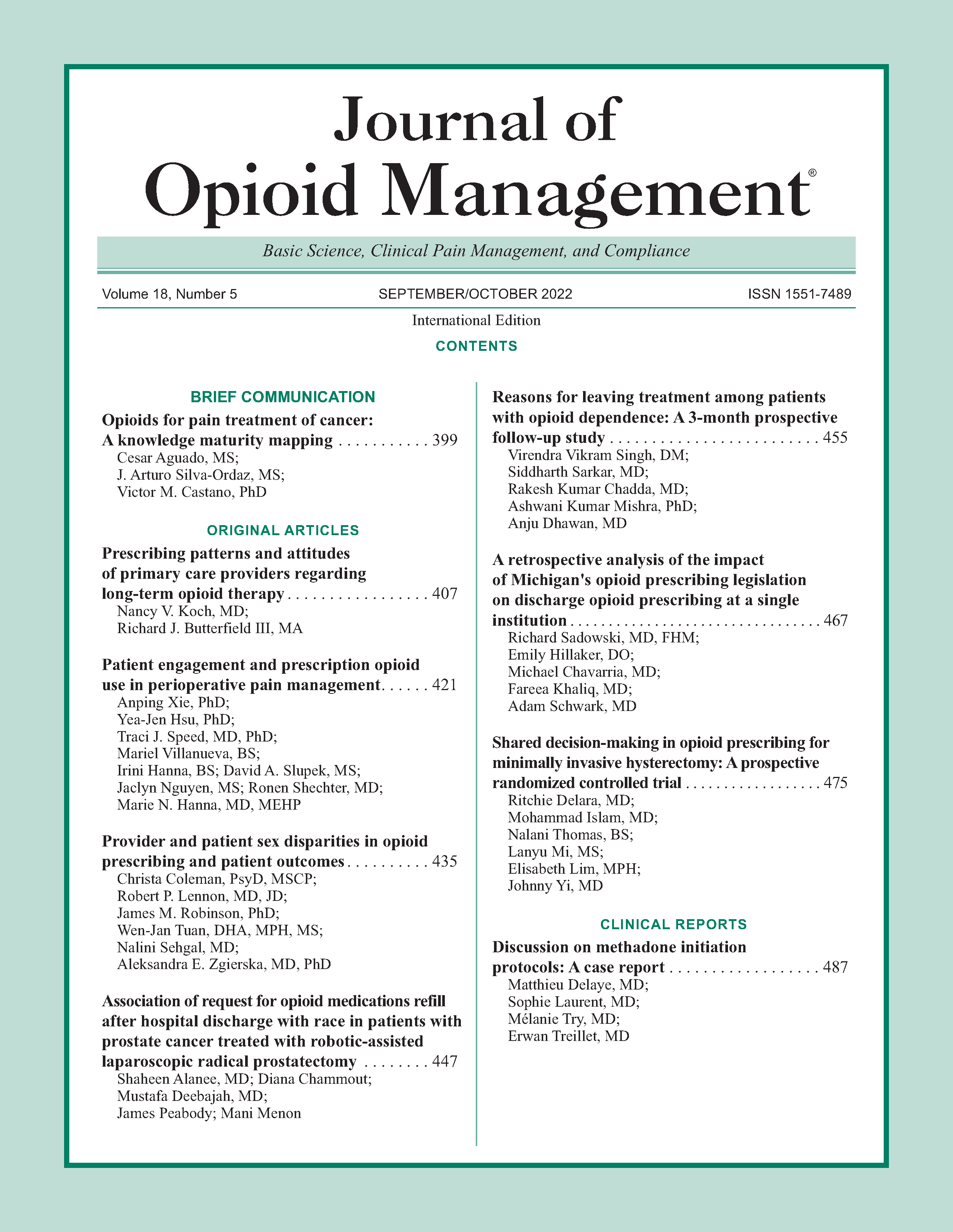
Patient engagement and prescription opioid use in perioperative pain management
DOI:
https://doi.org/10.5055/jom.2022.0736Keywords:
patient and family engagement, prescription opioid use, perioperative pain management, surveyAbstract
Objective: To examine (1) patient perceptions regarding their engagement and the engagement of their families in perioperative pain management, (2) demographic and clinical characteristics associated with perceived patient and family engagement, and (3) the association between perceived patient and family engagement and patient outcomes.
Design: A prospective, observational study.
Setting: The Personalized Pain Program (PPP) at the Johns Hopkins Hospital in Baltimore, Maryland.
Participants: Patients having more than one visit to the PPP.
Interventions: n/a.
Main outcome measures: Since the inception of the PPP, patients were surveyed prior to each clinic visit to assess their pain severity and interference using the Brief Pain Inventory. Starting August 22, 2018, two additional questions were added to the survey to assess patient perceptions of their engagement and the engagement of their families in perioperative pain management. In addition, electronic medical records were reviewed to collect data on daily opioid consumption during the first and last PPP visits presurgery and post-surgery.
Results: The final analysis included 511 survey responses from 155 patients. Perceived engagement of the patient in perioperative pain management improved over time (p < .001) and was significantly associated with reduction in prescription opioid consumption after surgery (coef = 12.7, SE = 5.8, p = .031).
Conclusions: Surgical patients and their family members should be actively engaged in perioperative pain management to improve prescription opioid use and the quality and safety of perioperative care.
References
Han B, Compton WM, Blanco C, et al.: Prescription opioid use, misuse, and use disorders in US adults: 2015 national survey on drug use and health. Ann Intern Med. 2017; 167(5): 293-301.
Rudd RA, Seth P, David F, et al.: Increases in drug and opioid-involved overdose deaths—United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016; 65(50-51): 1445-1452.
Hah JM, Bateman BT, Ratliff J, et al.: Chronic opioid use after surgery: Implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017; 125(5): 1733-1740.
Gan TJ, Habib AS, Miller TE, et al.: Incidence, patient satisfaction, and perceptions of post-surgical pain: Results from a US national survey. Curr Med Res Opin. 2014; 30(1): 149-160.
Sun EC, Darnall BD, Baker LC, et al.: Incidence of and risk factors for chronic opioid use among opioid-naive patients in the postoperative period. JAMA Intern Med. 2016; 176(9): 1286-1293.
Hanna MN, Speed TJ, Shechter R, et al.: An innovative perioperative pain program for chronic opioid users: An academic medical center's response to the opioid crisis. Am J Med Qual. 2019; 34(1): 5-13.
Mikhaeil J, Ayoo K, Clarke H, et al.: Review of the transitional pain service as a method of postoperative opioid weaning and a service aimed at minimizing the risk of chronic post-surgical pain. AIT. 2020; 52(2): 148-153.
Clarke JG, Martin RA, Gresko SA, et al.: The first comprehensive program for opioid use disorder in a US statewide correctional system. Am J Public Health. 2018; 108(10): 1323-1325.
Tiippana E, Hamunen K, Heiskanen T, et al.: New approach for treatment of prolonged postoperative pain: APS out-patient clinic. Scand J Pain. 2016; 12: 19-24.
American Society for Pain Management Nursing (ASPMN); Emergency Nurses Association (ENA); American College of Emergency Physicians (ACEP); American Pain Society (APS): Optimizing the treatment of pain in patients with acute presentations. Policy statement. Ann Emerg Med. 2010; 56(1): 77-79.
American Society of Anesthesiologists Task Force on Acute Pain Management: Practice guidelines for acute pain management in the perioperative setting: An updated report by the American society of anesthesiologists task force on acute pain management. Anesthesiology. 2012; 116(2): 248-273.
Chou R, Gordon DB, de Leon-Casasola OA, et al.: Management of postoperative pain: A clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine, and the American society of anesthesiologists' committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016; 17(2): 131-157.
Centers for Medicare & Medicaid Services (CMS) UDoHaHS: Opioid Misuse Strategy 2016. Baltimore, MD: CMS, 2017.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain–United States, 2016. JAMA. 2016; 315(15): 1624-1645.
Smith M, Saunders R, Stuckhardt L, et al.: Engaging Patients, Families, and Communities. Washington, DC: National Academic Press, 2013.
Matthias MS, Johnson NL, Shields CG, et al.: “I'm not gonna pull the rug out from under you”: Patient-provider communication about opioid tapering. J Pain. 2017; 18(11): 1365-1373.
Sullivan MD, Turner JA, DiLodovico C, et al.: Prescription opioid taper support for outpatients with chronic pain: A randomized controlled trial. J Pain. 2017; 18(3): 308-318.
Darnall BD, Ziadni MS, Stieg RL, et al.: Patient-centered prescription opioid tapering in community outpatients with chronic pain. JAMA Intern Med. 2018; 178(5): 707-708.
Pergolizzi JV, Varrassi G, Paladini A, et al.: Stopping or decreasing opioid therapy in patients on chronic opioid therapy. Pain Ther. 2019; 8(2): 163-176.
Shechter R, Speed TJ, Blume E, et al.: Addressing the opioid crisis one surgical patient at a time: Outcomes of a novel perioperative pain program. Am J Med Qual. 2020; 35(1): 5-15.
Tan G, Jensen MP, Thornby JI, et al.: Validation of the brief pain inventory for chronic nonmalignant pain. J Pain. 2004; 5(2): 133-137.
Cleeland CS: The brief pain inventory user guide. Available at https://www.mdanderson.org/documents/Departments-and-Divisions/Symptom-Research/BPI_UserGuide.pdf. Accessed February 24, 2021.
Hair JF, Babin BJ, Anderson RE, et al.: Multivariate Data Analysis. 8th ed. London, UK: Cengage Learning EMEA, 2018.
Yajnik M, Hill JN, Hunter OO, et al.: Patient education and engagement in postoperative pain management decreases opioid use following knee replacement surgery. Patient Educ Couns. 2019; 102(2): 383-387.
Turk DC, Kerns RD: Health, Illness, and Families: A Life-Span Perspective. New York, NY: John Wiley & Sons, 1985.
Ojeda B, Salazar A, Duenas M, et al.: The impact of chronic pain: The perspective of patients, relatives, and caregivers. Fam Syst Health. 2014; 32(4): 399-407.
Bjornnes AK, Moons P, Parry M, et al.: Experiences of informal caregivers after cardiac surgery: A systematic integrated review of qualitative and quantitative studies. BMJ Open. 2019; 9(11): e032751.
Flor H, Turk DC, Rudy TE: Relationship of pain impact and significant other reinforcement of pain behaviors: The mediating role of gender, marital status and marital satisfaction. Pain. 1989; 38(1): 45-50.
Block AR, Kremer EF, Gaylor M: Behavioral treatment of chronic pain: The spouse as a discriminative cue for pain behavior. Pain. 1980; 9(2): 243-252.
Flor H, Turk DC, Rudy TE: Pain and families. II. Assessment and treatment. Pain. 1987; 30(1): 29-45.
Turk DC, Flor H: Pain greater than pain behaviors: The utility and limitations of the pain behavior construct. Pain. 1987; 31(3): 277-295.
Turk DC, Kerns RD, Rosenberg R: Effects of marital interaction on chronic pain and disability: Examining the down side of social support. Rehabil Psychol. 1992; 37(4): 259-274.
Sullivan MD, Vowles KE: Patient action: As means and end for chronic pain care. Pain. 2017; 158(8): 1405-1407.
Burley G, Torres L, Heligman J: Improving the patient experience following total knee and total hip arthroplasty: A practice development project. J Nurs Care Qual. 2020; 35(2): 171-176.
Xie A, Carayon P: A systematic review of human factors and ergonomics (HFE)-based healthcare system redesign for quality of care and patient safety. Ergonomics. 2015; 58(1): 33-49.
Jayakumar P, Teunis T, Vranceanu AM, et al.: The impact of a patient's engagement in their health on the magnitude of limitations and experience following upper limb fractures. Bone Joint J. 2020; 102-B(1): 42-47.
US Department of Health and Human Services: Pain Management Best Practices Inter-Agency Task Force Report: Updates, Gaps, Inconsistencies, and Recommendations. Washington, DC: US Department of Health and Human Services, 2019.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.