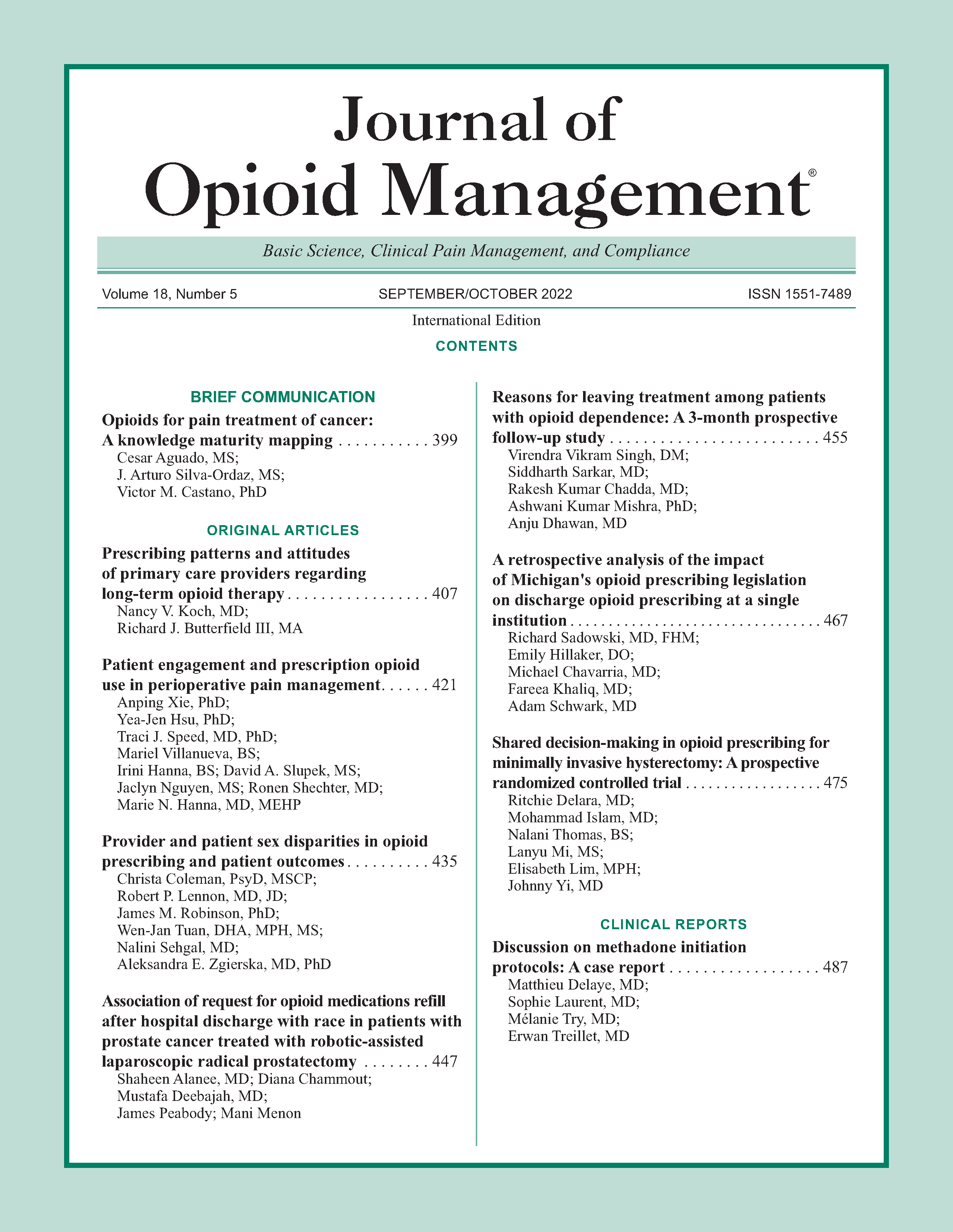
Provider and patient sex disparities in opioid prescribing and patient outcomes
DOI:
https://doi.org/10.5055/jom.2022.0737Keywords:
opioid, pain, sex disparitiesAbstract
Objective: To assess sex disparities in opioid prescribing practices and patient outcomes.
Design: A retrospective cross-sectional study.
Setting: Thirty-three primary care clinics in an academic health system.
Participants: 2,738 adults prescribed 10+ outpatient opioid prescriptions within 12 months.
Main outcome measure(s): Patient and primary care provider (PCP) sex-based differences in clinical outcomes, opioid prescribing, and rates of adherence to guideline-concordant opioid prescribing practices.
Results: Female PCPs were more likely (p < 0.001) to prescribe lower morphine-equivalent daily dose (MEDD) of opioids and complete risk assessment for opioid misuse than male PCPs. PCPs did not differ by sex in adherence rates to controlled substance agreements, urine drug, depression screening, or opioid-benzodiazepine coprescribing.
Female patients were more likely (all p ≤ 0.01) to be screened for opioid misuse, treated with lower MEDD, receive opioid-benzodiazepine coprescriptions, have higher pain interference, anxiety and depression diagnoses, and have an overdose diagnosis; they were less likely (all p < 0.001) to report alcohol use or have an alcohol use disorder diagnosis and utilized health care at higher rates than male patients.
Conclusions: Sex differences were found in clinician opioid-prescribing practices and adherence to opioid prescribing guidelines and patient characteristics associated with long-term opioid therapy. Strategies to identify sex-related disparities and enhance guideline-concordant opioid prescribing and monitoring could contribute to improved patient care, and clinical and safety outcomes.
References
Zelaya CE, Dahlhamer JM, Lucas JW, et al.: Chronic Pain and High-Impact Chronic Pain among US Adults. NCHS Data Brief no. 390. Hyattsville, MD: National Center for Health Statistics, 2020.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States. MMWR Recomm Rep. 2016: 54(No. RR-1): 1-49. DOI: 10.15585/mmwr.rr6501e1.
Manchikanti L, Abdi S, Atluri S, et al.: American society of interventional pain physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part I–evidence assessment. Pain Phys. 2012; 15(3 Suppl.): S1-65.
Manchikanti L, Abdi S, Atluri S, et al.: American society of interventional pain physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2–guidance. Pain Phys. 2012; 15(3 Suppl.): S67-116.
Chou R, Deyo R, Devine B, et al.: The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain. Evidence Report/Technology Assessment No. 218. (Prepared by the Pacific Northwest Evidence-based Practice Center under Contract No. 290-2012-00014-I.) AHRQ Publication No. 14-E005-EF. Rockville, MD: Agency for Healthcare Research and Quality, 2014. Available at http://www.effectivehealthcare.ahrq.gov/ehc/products/557/1971/chronic-pain-opioid-treatmentreport-141205.pdf. Accessed February 20, 2021.
Volkow ND, Jones EB, Einstein EB, et al.: Prevention and treatment of opioid misuse and addiction: A review. JAMA Psychiatry. 2019; 76: 208.
Rose AJ, Bernson D, Chui KKH, et al.: Potentially inappropriate opioid prescribing, overdose, and mortality in Massachusetts, 2011-2015. J Gen Intern Med. 2018; 33(9): 1512-1519.
Cochella S, Bateman K: Provider detailing: An intervention to decrease prescription opioid deaths in Utah. Pain Med. 2011; 12(Suppl. 2): S73-S76.
Franklin GM, Mai J, Turner J, et al.: Bending the prescription opioid dosing and mortality curves: Impact of the Washington state opioid dosing guideline. Am J Ind Med. 2012; 55(4): 325-331.
Chen JH, Hom J, Richman I, et al.: Effect of opioid prescribing guidelines in primary care. Medicine (Baltimore). 2016; 95(35): E4760.
Fox TR, Li J, Stevens S, et al.: A performance improvement prescribing guideline reduces opioid prescriptions for emergency department dental pain patients. Ann Emerg Med. 2013; 62(3): 237-240.
Quanbeck A, Brown RT, Zgierska AE, et al.: A randomized matched-pairs study of feasibility, acceptability, and effectiveness of systems consultation: A novel implementation strategy for adopting clinical guidelines for opioid prescribing in primary care. Implementation Sci. 2018; 13(1): 21.
Levy B, Paulozzi L, Mack KA, et al.: Trends in opioid analgesic-prescribing rates by specialty, US, 2007-2012. Am J Prev Med. 2015; 49(3): 409-413.
Shiffman RN, Dixon J, Brandt C, et al.: The GuideLine implementability appraisal (GLIA): Development of an instrument to identify obstacles to guideline implementation. BMC Med Inform Decis Mak. 2005; 5: 23.
Grimshaw JM, Thomas RE, MacLennan G, et al.: Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004; 8(6): iii-iv, 1-72.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States. MMWR Recomm Rep. 2016; 65(1): 1-49.
Zgierska AE, Robinson JM, Lennon RP, et al.: Increasing system-wide implementation of opioid prescribing guidelines in primary care: Findings from a non-randomized stepped-wedge quality improvement project. BMC Fam Pract. 2020; 21: 245. DOI: 10.1186/s12875-020-01320-9.
Cron DC, Lee JS, Dupree JM, et al.: Provider characteristics associated with outpatient opioid prescribing after surgery. Ann Surg. 2020; 271(4): 680-685. DOI: 10.1097/SLA.0000000000003013.
Lui LMW, Lee Y, Lipsitz O, et al.: The influence of prescriber and patient gender on the prescription of benzodiazepines: Results from the Florida Medicaid dataset. CNS Spectr. 2021; 1-5. DOI: 10.1017/S1092852921000055.
Darnall BD, Stacey BR, Chou R: Medical and psychological risks and consequences of long-term opioid therapy in women. Pain Med. 2012; 13(9): 1181-1211. DOI: 10.1111/j.1526-4637.2012.01467.x.
Centers for Disease Control and Prevention (CDC): Opioid overdose. Nonfatal overdoses: All opioids. Available at https://www.cdc.gov/drugoverdose/data/nonfatal/nonfatal-opioids.html. Accessed April 3, 2021.
Mattson CL, Tanz LJ, Quinn K, et al.: Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021; 70: 202-207. DOI: 10.15585/mmwr.mm7006a4.
CDC: US opioid dispensing rate maps, 2021. Available at https://www.cdc.gov/drugoverdose/rxrate-maps/index.html. Accessed November 4, 2021.
KFF analysis of Centers for Disease Control and Prevention (CDC): National Center for Health Statistics. Multiple Cause of Death 1999-2019 on CDC WONDER Online Database, released 2021. Available at http://wonder.cdc.gov/mcd-icd10.html. Accessed April 3, 2021.
Deyo RA, Smith DH, Johnson ES, et al.: Opioids for back pain patients: Primary care prescribing patterns and use of services. J Am Board Fam Med. 2011; 24(6): 717-727.
Quanbeck A, Brown RT, Zgierska A, et al.: Systems consultation: Protocol for a novel implementation strategy designed to promote evidence-based practice in primary care. Health Res Policy Sys. 2016; 14: 8. DOI: 10.1186/s12961-016-0079-2.
Tuan W, Sehgal N, Zgierska AE: Using electronic health record's data to assess daily dose of opioids prescribed for outpatients with chronic non-cancer pain. Family Med Community Health. 2021; 9(Suppl. 1): e001277. DOI: 10.1136/fmch-2021-001277.
Zgierska AE, Vidaver RM, Smith P, et al.: Enhancing system-wide implementation of opioid prescribing guidelines in primary care: Protocol for a stepped-wedge quality improvement project. BMC Health Serv Res. 2018; 18: 415. DOI: 10.1186/s12913-018-3227-2.
US Department of Health and Human Services: Pain management best practices inter-agency task force report: Updates, gaps, inconsistencies, and recommendations. US Department of Health and Human Services website. 2019. Available at https://www.hhs.gov/ash/advisory-committees/pain/reports/index.html. Accessed January 8, 2021.
Kroenke K, Spitzer RL, Williams JB: The patient health questionnaire-2: Validity of a two-item depression screener. Med Care. 2003; 41(11): 1284-1292. DOI: 10.1097/01.MLR.0000093487.78664.3C.
Kroenke K, Spitzer RL, Williams JB: The PHQ-9: Validity of a brief depression severity measure. Research support, non-US gov't validation studies. J Gen Intern Med. 2001; 16(9): 606-613.
Belgrade MJ, Schamber CD, Lindgren BR: The DIRE score: Predicting outcomes of opioid prescribing for chronic pain. J Pain. 2006; 7(9): 671-681. DOI: 10.1016/j.jpain.2006.03.001.
US Department of Health and Human Services, Guidance Portal: Opioid oral morphine milligram equivalent (MME) conversion factors table for prescription drug coverage. Issued by Centers for Medicare & Medicaid Services (CMS). 2020. Available at https://www.hhs.gov/guidance/document/opioidoral-morphine-milligram-equivalent-mme-conversion-factors-0. Accessed April 30, 2021.
Data Resources: Centers for disease control and prevention. 2021. Available at https://www.cdc.gov/drugoverdose/resources/data.html. Accessed April 29, 2021.
Korff Jensen VM, Karoly MP: Assessing global pain severity by self-report in clinical and health services research. Spine. 2000; 25(24): 3140-3151.
Rovner GS, Sunnerhagen KS, Björkdahl A, et al.: Chronic pain and sex-differences; women accept and move, while men feel blue. PLoS One. 2017; 12: E0175737. DOI: 10.1371/journal.pone.0175737.
Turk DC, Rudy TE: Towards a comprehensive assessment of chronic pain patients. Behav Res Ther. 1987; 25(4): 237-249.
McIntyre RS, Chen VC, Lee Y, et al.: The influence of prescriber and patient gender on the prescription of benzodiazepines: Evidence for stereotypes and biases? Soc Psychiatry Psychiatr Epidemiol. 2021; 56: 1083-1089. DOI: 10.1007/s00127-020-01989-4.
Olfson M, Wall M, Wang S, et al.: Risks of fatal opioid overdose during the first year following nonfatal overdose. Drug Alcohol Dependence. 2018; 190: 112-119. DOI: 10.1016/j.drugalcdep.2018.06.004.
Weisse CS, Sorum PC, Dominguez RE: The influence of gender and race on physicians' pain management decisions. J Pain. 2003; 4(9): 505-510. DOI: 10.1016/j.jpain.2003.08.002.
Baumhäkel M, Müller U, Böhm M: Influence of gender of physicians and patients on guideline-recommended treatment of chronic heart failure in a cross-sectional study. Eur J Heart Fail. 2009; 11(3): 299-303. DOI: 10.1093/eurjhf/hfn041.
Bertakis KD, Azari R: Patient-centered care: The influence of patient and resident physician gender and gender concordance in primary care. J Womens Health (Larchmt). 2012; 21(3): 326-333. DOI: 10.1089/jwh.2011.2903.
Safdar B, Heins A, Homel P, et al.: Impact of physician and patient gender on pain management in the emergency department—A multicenter study. Pain Med. 2009; 10(2): 364-372. DOI: 10.1111/j.1526-4637.2008.00524.x.
Chen EH, Shofer FS, Dean AJ, et al.: Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med. 2008; 15(5): 414-418.
Schäfer G, Prkachin KM, Kaseweter KA, et al.: Health care providers’ judgments in chronic pain: The influence of gender and trustworthiness. Pain. 2016; 157(8): 1618-1625.
Haegerich TM, Jones CM, Cote P, et al.: Evidence for state, community and systems-level prevention strategies to address the opioid crisis. Drug Alcohol Dependence. 2019; 204: 107563. DOI: 10.1016/j.drugalcdep.2019.107563.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.