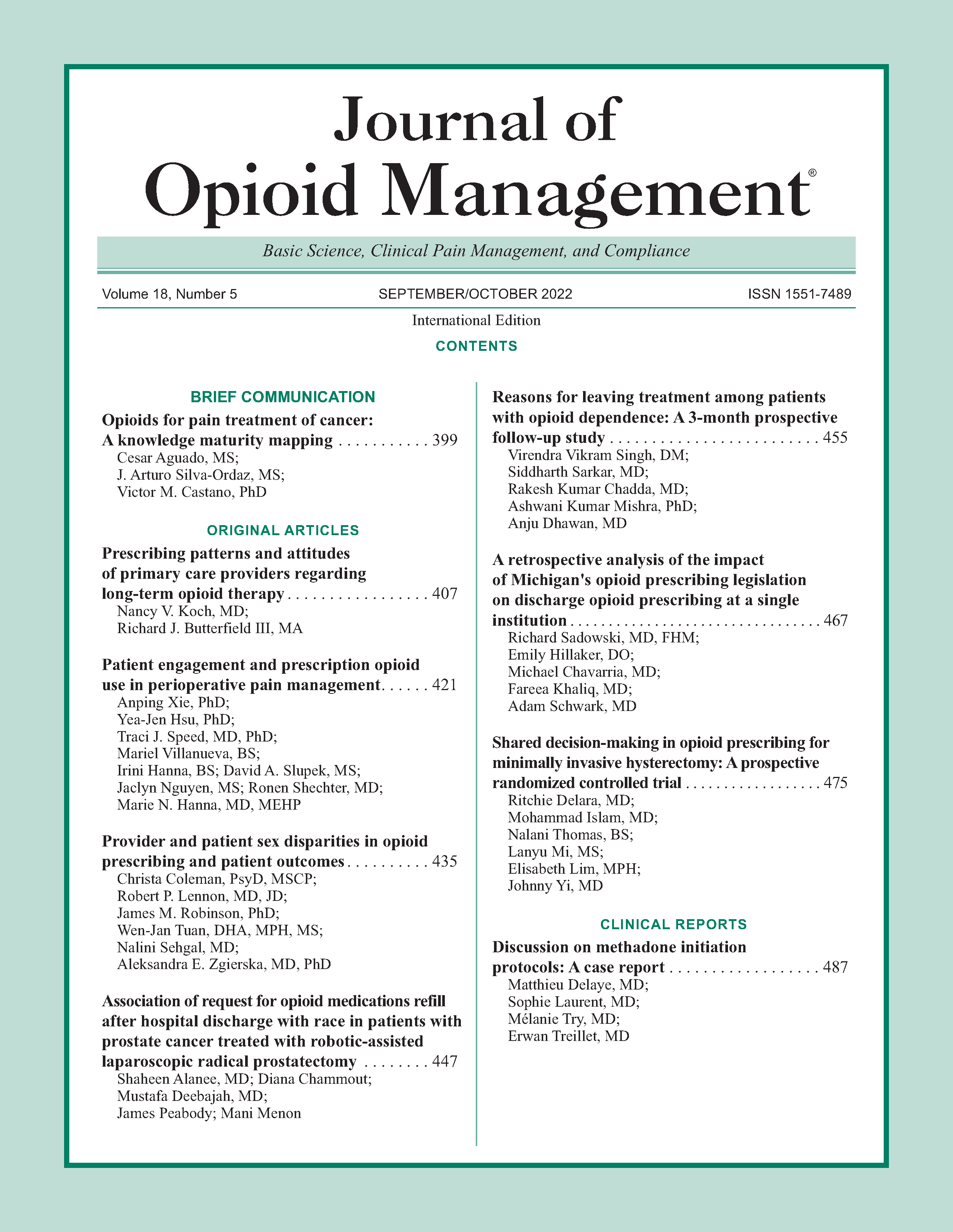
Shared decision-making in opioid prescribing for minimally invasive hysterectomy: A prospective randomized controlled trial
DOI:
https://doi.org/10.5055/jom.2022.0741Keywords:
individualized prescribing, minimally invasive hysterectomy, opioid utilization, patient satisfaction, perioperative pain management, post-operative painAbstract
Objective: To determine the impact of shared decision-making in postsurgical opioid prescribing in women who underwent minimally invasive (MIS) hysterectomy.
Design: A randomized controlled trial.
Setting: A single, tertiary care, academic center.
Patients and participants: From January 2019 through April 2020, 73 women aged 18 years and older who had a planned MIS hysterectomy with the Department of Gynecology were enrolled into the study (36 in the standard arm and 37 in the patient-directed arm).
Interventions: Participants were assigned either to the standard arm (30 tablets) or patient-directed arm (0–30 tablets) of oxycodone 5 mg.
Main outcome measures: The primary outcome was the percentage of excess opioid tablets, calculated by the number of unused tablets divided by the number of tablets prescribed. Secondary outcomes included total opioid tablets used, frequency of obtaining additional opioid tablets after discharge, frequency of unscheduled post-operative visits, and patient satisfaction with number of opioid tablets prescribed.
Results: Age, race, and body mass index did not differ between groups. Hysterectomies were performed via laparoscopy (16.9 percent), robotic-assisted laparoscopy (38.5 percent), and vaginal routes (44.6 percent). The median (IQR) number of oxycodone prescribed in the patient-directed arm was 15.0 (12.0 and 24.0) tablets. The standard arm had a greater percentage of excess oxycodone tablets 73.6 percent (0.03) than the patient-directed arm 56.3 percent (0.03, p < .01). However, there was no difference in the total number of oxycodone used by patients in the standard (mean 7.9 [0.5] tablets) and patient-directed arms (mean 8.4 [0.5] tablets, p = .50). The mean number of oxycodone used for the entire cohort was 8.1 (0.4) tablets.
Conclusions: Shared decision-making significantly decreased the percent of excess oxycodone tablets but did not decrease the total number of oxycodone tablets used in patients undergoing MIS hysterectomy. Patients used about 22 tablets less than the standard 30 tablets prescribed.
References
Upp LA, Waljee JF: The opioid epidemic. Clin Plast Surg. 2020; 47(2): 181-190.
As-Sanie S, Till SR, Mowers EL, et al.: Opioid prescribing patterns, patient use, and postoperative pain after hysterectomy for benign indications. Obstet Gynecol. 2017; 130(6): 1261-1268.
Chou R, Gordon DB, de Leon-Casasola OA, et al.: Management of postoperative pain: A clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016; 17(2): 131-157.
Griffith KC, Clark NV, Zuckerman AL, et al.: Opioid prescription and patient use after gynecologic procedures: A survey of patients and providers. J Minim Invasive Gynecol. 2018; 25(4): 684-688.
Bartels K, Mayes LM, Dingmann C, et al.: Opioid use and storage patterns by patients after hospital discharge following surgery. PLoS One. 2016; 11(1): e0147972.
Kennedy-Hendricks A, Gielen A, McDonald E, et al.: Medication sharing, storage, and disposal practices for opioid medications among US adults. JAMA Intern Med. 2016; 176(7): 1027-1029.
Waljee JF, Li L, Brummett CM, et al.: Iatrogenic opioid dependence in the United States: Are surgeons the gatekeepers? Ann Surg. 2017; 265(4): 728-730.
Osmundson SS, Raymond BL, Kook BT, et al.: Individualized compared with standard postdischarge oxycodone prescribing after cesarean birth: A randomized controlled trial. Obstet Gynecol. 2018; 132(3): 624-630.
Prabhu M, Dubois H, James K, et al.: Implementation of a quality improvement initiative to decrease opioid prescribing after cesarean delivery. Obstet Gynecol. 2018; 132(3): 631-636.
Prabhu M, McQuaid-Hanson E, Hopp S, et al.: A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017; 130(1): 42-46.
Vilkins AL, Sahara M, Till SR, et al.: Effects of shared decision making on opioid prescribing after hysterectomy. Obstet Gynecol. 2019; 134(4): 823-833.
Harris PA, Taylor R, Minor BL, et al.: The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019; 95: 103208.
Harris PA, Taylor R, Thielke R, et al.: Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42(2): 377-381.
Johnson N, Barlow D, Lethaby A, et al.: Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2006; 2: CD003677.
Martinez V, Beloeil H, Marret E, et al.: Non-opioid analgesics in adults after major surgery: Systematic review with network meta-analysis of randomized trials. Br J Anaesth. 2017; 118(1): 22-31.
Ong CK, Seymour RA, Lirk P, et al.: Combining paracetamol (acetaminophen) with nonsteroidal anti-inflammatory drugs: A qualitative systematic review of analgesic efficacy for acute postoperative pain. Anesth Analg. 2010; 110(4): 1170-1179.
Lamvu G: Role of hysterectomy in the treatment of chronic pelvic pain. Obstet Gynecol. 2011; 117(5): 1175-1178.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.