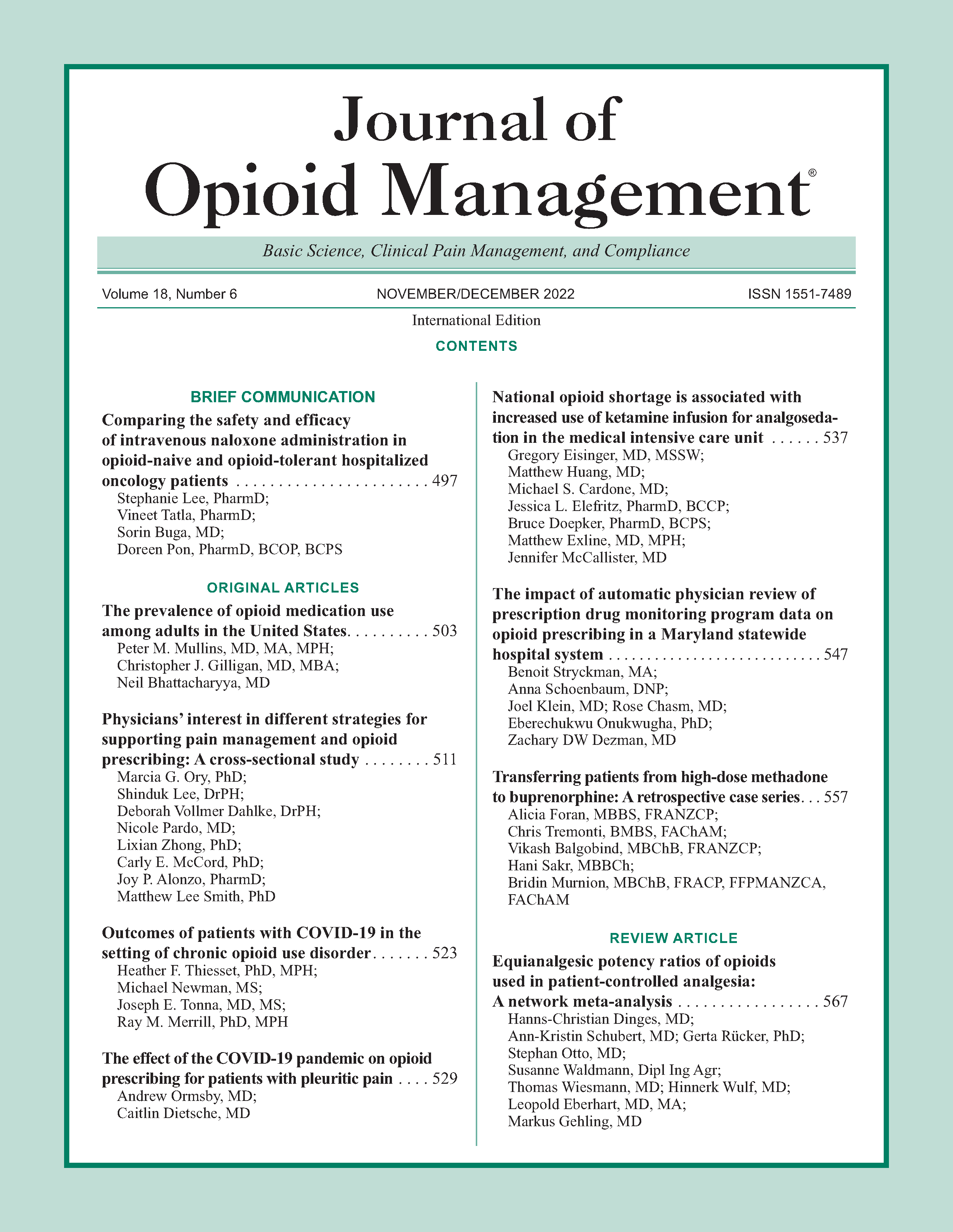
Transferring patients from high-dose methadone to buprenorphine: A retrospective case series
DOI:
https://doi.org/10.5055/jom.2022.0752Keywords:
buprenorphine/naloxone, methadone, transferAbstract
Objective: Transferring from methadone to buprenorphine can be difficult, particularly at higher methadone doses. Precipitated withdrawal (PW) and severe opioid withdrawal can compromise transfers and limited data guide high-dose transfers. This study describes processes and outcomes of transfers to buprenorphine from methadone.
Design: A retrospective case series of transfers from methadone to buprenorphine.
Setting: Two elective, voluntary, specialized in-patient drug and alcohol facilities in Sydney, New South Wales, Australia.
Participants: All admissions between July 1, 2015 and April 30, 2019 were screened using routinely collected coding data. The medical record was reviewed to identify subjects meeting the inclusion criteria of daily methadone use for at least 1 month, age > 18, and a treatment plan that included transfer from methadone to buprenorphine. Data were extracted on methadone dose, transfer medications, time to buprenorphine initiation, and transfer outcome.
Interventions: Subjects were transferred via two methods: morphine bridged and nonbridged.
Main outcome measure: The primary outcome measure was successful transition to buprenorphine.
Results: Seventy-one subjects met inclusion criteria, of whom 62 initiated buprenorphine and 53 discharged on buprenorphine. Longer delay to buprenorphine initiation was seen with higher methadone doses. The highest daily methadone dose in subjects completing transfer was 180 mg. Outcomes with morphine bridging, using a steady state methadone: morphine ratio of 1:4, were similar to direct transfer. Only one subject discontinued buprenorphine because of PW.
Conclusions: Transfer from high doses of methadone to buprenorphine can be achieved with high success rates in the in-patient setting.
References
Australian Institute of Health and Welfare: National Opioid Pharmacotherapy Statistics Annual Data Collection. Cat. no. PHE 266. Canberra: AIHW, 2021. Available at https://www.aihw.gov.au/reports/alcohol-other-drug-treatment-services/nationalopioid-pharmacotherapy-statistics/contents/summary. Accessed April 7, 2021.
NSW Health: NSW Clinical Guidelines: Treatment of Opioid Dependence. 2018. Available at https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2018_019.pdf. Accessed December 28, 2020.
Clinical Guidelines on Drug Misuse and Dependence Update 2017; Independent Expert Working Group (2017): Drug Misuse and Dependence: UK Guidelines on Clinical Management. London: Department of Health, 2017.
National Guidelines for Medication-Assisted Treatment of Opioid Dependence: Department of Health and Ageing 2014. Available at https://www.clinicalguidelines.gov.au/portal/2437/national-guidelines-medication-assisted-treatment-opioid-dependence. Accessed April 10, 2021.
Lintzeris N, Monds LA, Rivas C, et al.: Transferring patients from methadone to buprenorphine: The feasibility and evaluation of practice guidelines. J Addict Med. 2018; 12(3): 234-240.
Therapeutic Goods Administration: Australian public assessment report for buprenorphine. 2019. Available at https://www.tga.gov.au/sites/default/files/auspar-buprenorphine-191106.pdf. Accessed April 10, 2021.
Lintzeris N, Hayes V, Arunogiri S: Interim guidance for the delivery of medication assisted treatment of opioid dependence in response to COVID-19: A national response. 2020. Available at https://www.racp.edu.au/docs/default-source/news-and-events/covid-19/interim-guidance-delivery-of-medication-assisted-treatment-of-opiod-dependence-covid-19.pdf?sfvrsn=e36eeb1a_4. Accessed April 17, 2021.
Oretti R: A retrospective evaluation of inpatient transfer from high-dose methadone to buprenorphine substitution therapy. J Subst Abuse Treat. 2015; 57: 102-105.
Wesson DR, Ling W: The clinical opiate withdrawal scale (COWS). J Psychoact Drugs. 2003; 35(2): 253-259.
Whitley SD, Sohler NL, Kunins HV, et al.: Factors associated with complicated buprenorphine inductions. J Subst Abuse Treat. 2010; 39(1): 51-57.
Bishop B, Gilmour J, Deering D: Readiness and recovery: Transferring between methadone and buprenorphine/naloxone for the treatment of opioid use disorder. Int J Mental Health Nurs. 2019; 28(1): 226-236.
Azar P, Nikoo M, Miles I: Methadone to buprenorphine/naloxone induction without withdrawal utilizing transdermal fentanyl bridge in an inpatient setting-Azar method. Am J Addict. 2018; 27(8): 601-604.
Wong JSH, Nikoo M, Westenberg JN, et al.: Comparing rapid micro-induction and standard induction of buprenorphine/naloxone for treatment of opioid use disorder: Protocol for an open-label, parallel-group, superiority, randomized controlled trial. Addict Sci Clin Pract. 2021; 16(1): 11.
Randhawa PA, Brar R, Nolan S: Buprenorphine-naloxone “microdosing”: An alternative induction approach for the treatment of opioid use disorder in the wake of North America's increasingly potent illicit drug market. Can Med Assoc J. 2020; 192(3): E73.
Ahmed S, Bhivandkar S, Lonergan BB, et al.: Microinduction of buprenorphine/naloxone: A review of the literature. Am J Addict. 2021; 30(4): 305-315.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.