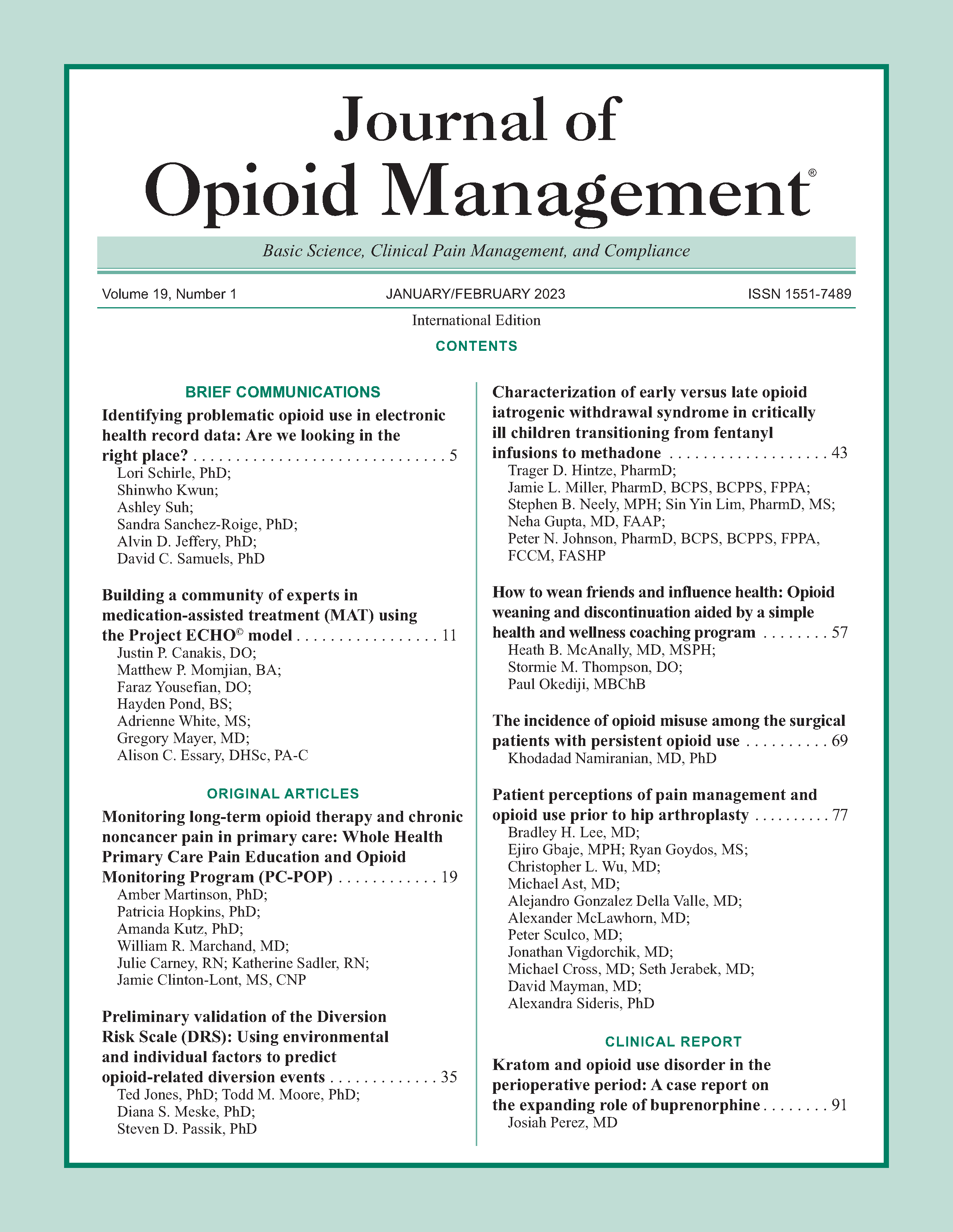
How to wean friends and influence health: Opioid weaning and discontinuation aided by a simple health and wellness coaching program
DOI:
https://doi.org/10.5055/jom.2023.0759Keywords:
chronic opioid use, opioid weaning, opioid discontinuation, health and wellness coaching, pain neuroscience education, multidisciplinary, therapeutic allianceAbstract
Objective: To evaluate whether a simple health and wellness coaching (HWC) program embedded within routine clinical practice resulted in improved opioid weaning and discontinuation.
Design: Retrospective double cohort study comparing longitudinal opioid use data and numeric pain scale ratings for patients in each group.
Setting: Single noninstitutional subspecialty pain management practice.
Participants: Twenty (daily opioid using) patients undergoing a multifocal HWC program with integrated pain neuroscience education (PNE) compared to 20 age- and gender-matched (daily opioid using) patients undergoing usual care.
Intervention: A systematized series of interactive self-management topics/lessons on basic health topics pertinent to chronic pain, eg, posture, mobility, nutrition, sleep, stress management, and PNE.
Main outcome measures: Daily morphine milligram equivalents (MMEs) trajectory and discontinuation success (hypothesis and outcome measure formulated before data collection); numeric pain scale rating trajectory (hypothesis and outcome measure formulated after data collection).
Results: MME decrease was significantly greater among cases (93.5 percent) than controls (50 percent; p = 0.004) as was discontinuation of opioids (30 percent vs 0). Cases reported decreased longitudinal 10-digit pain scale rating (–0.8) compared to controls (+0.1) without statistical significance.
Conclusions: Providing simple and salient HWC including PNE within pain management can significantly improve opioid weaning and discontinuation while mitigating pain.
References
Centers for Disease Control and Prevention: CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR. 2016; 65(1): 1-49.
Veterans Administration/Department of Defense: VA/DoD Clinical Practice Guideline for Management of Opioid Therapy for Chronic Pain. Washington, DC: Veterans Administration, 2010. Available at http://www.va.gov/painmanagement/docs/cpg_opioidtherapy_fulltext.pdf. Accessed January 14, 2022.
Manchikanti L, Kaye AM, Knezevic NN, et al.: Responsible, safe, and effective prescription of opioids for chronic non-cancer pain: American Society of Interventional Pain Physicians (ASIPP) guidelines. Pain Physician. 2017; 20(2S): S3-S92.
Goesling J, DeJonckheere M, Pierce J, et al.: Opioid cessation and chronic pain: Perspectives of former opioid users. Pain. 2019; 160(5): 1131-1145. DOI: 10.1097/j.pain.0000000000001493.PMID: 30889052.
Frank JW, Levy C, Matlock DD, et al.: Patients’ perspectives on tapering of chronic opioid therapy: A qualitative study. Pain Med. 2016; 17: 1838-1847.
Berna C, Kulich RJ, Rathmell JP: Tapering long-term opioid therapy in chronic noncancer pain: Evidence and recommendations for everyday practice. Mayo Clin Proc. 2015; 90(6): 828-842. DOI: 10.1016/j.mayocp.2015.04.003.
Robinson JP, Dansie EJ, Wilson HD, et al.: Attitudes and beliefs of working and work-disabled people with chronic pain prescribed long-term opioids. Pain Med. 2015; 16(7): 1311-1324. DOI: 10.1111/pme.12770.
Matthias MS, Johnson NL, Shields CG, et al.: “I'm not gonna pull the rug out from under you”: Patient-provider communication about opioid tapering. J Pain. 2017; 18(11): 1365-1373. DOI: 10.1016/j.jpain.2017.06.008.
Huffman KL, Sweis GW, Gase A, et al.: Opioid use 12 months following interdisciplinary pain rehabilitation with weaning. Pain Med. 2013; 14(12): 1908-1917. DOI: 10.1111/pme.12201.
Frank JW, Lovejoy TI, Becker WC, et al.: Patient outcomes in dose reduction or discontinuation of long-term opioid therapy: A systematic review. Ann Intern Med. 2017; 167(3): 181-191. DOI: 10.7326/M17-0598.
US Department of Health and Human Services: HHS guide for clinicians on the appropriate dosage reduction or discontinuation of long-term opioid analgesics. Available at https://www.hhs.gov/opioids/sites/default/files/2019-10/Dosage_Reduction_Discontinuation.pdf. Accessed November 29, 2020.
Darnall BD, Ziadni MS, Stieg RL, et al.: Patient-centered prescription opioid tapering in community outpatients with chronic pain. JAMA Intern Med. 2018; 178(5): 707-708.
Sud A, Armas A, Cunningham H, et al.: Multidisciplinary care for opioid dose reduction in patients with chronic noncancer pain: A systematic realist review. PLoS One. 2020; 15(7): e0236419. DOI: 10.1371/journal.pone.0236419.
Eccleston C, Fisher E, Thomas KH, et al.: Interventions for the reduction of prescribed opioid use in chronic noncancer pain. Database Syst Rev. 2017; 11(11): CD010323. DOI: 10.1002/14651858.CD010323.pub3.
Canlas BR, Dawson TC, Hollrah LN, et al.: Restoring function in veterans with complex chronic pain. Fed Pract. 2017; 34(10): 42-47.
Darnall BD, Mackey SC, Lorig K, et al.: Comparative effectiveness of cognitive behavioral therapy for chronic pain and chronic pain self-management within the context of voluntary patient-centered prescription opioid tapering: The EMPOWER study protocol. Pain Med. 2020; 21(8): 1523-1531. DOI: 10.1093/pm/pnz285.
Cummings SR, Ernster V, Hulley SB: Designing a new study: I. Cohort studies. In Hulley SB, Cummings SR (eds.): Designing Clinical Research. Baltimore: Wilkins & Wilkins, 1988: 63-74.
Available at https://www.cms.gov/Medicare/Prescription-Drug-coverage/PrescriptionDrugCovContra/Downloads/Opioid-Morphine-EQ-Conversion-Factors-Aug-2017.pdf. Accessed May 15, 2021.
Fudin J, Raouf M, Wegrzyn EL, et al.: Safety concerns with the centers for disease control opioid calculator. J Pain Res. 2017; 11: 1-4.
Available at https://pubchem.ncbi.nlm.nih.gov/compound/Tapentadol#section=Pharmacology-and-Biochemistry. Accessed May 15, 2021.
McNerney NA, Losensky MJ, Lash MM, et al.: Low theoretical fidelity hinders the research on health coaching for opioid reduction: A systematic review of randomized controlled trials. PLoS One. 2020; 15(10): e0241434. DOI: 10.1371/journal.pone.0241434.
Rethorn ZD, Pettitt RW, Dykstra E, et al.: Health and wellness coaching positively impacts individuals with chronic pain and pain-related interference. PLoS One. 2020; 15(7): e0236734. DOI: 10.1371/journal.pone.0236734.
Hackshaw KV, Plans-Pujolras M, Rodriguez-Saona LE, et al.: A pilot study of health and wellness coaching for fibromyalgia. BMC Musculoskelet Disord. 2016; 17(1): 457. DOI: 10.1186/s12891-016-1316-0.
Rogers AH, Garey L, Raines AM, et al.: Anxiety sensitivity and opioid use motives among adults with chronic low back pain. Exp Clin Psychopharmacol. 2020; DOI: 10.1037/pha0000381.
Martel MO, Finan PH, McHugh RK, et al.: Day-to-day pain symptoms are only weakly associated with opioid craving among patients with chronic pain prescribed opioid therapy. Drug Alcohol Depend. 2016; 162: 130-136. DOI: 10.1016/j.drugalcdep.2016.02.047.
Malinoff HL, Barkin RL, Wilson G: Sublingual buprenorphine is effective in the treatment of chronic pain syndrome. Am J Ther. 2005; 12(5): 379-384.
Daitch J, Frey ME, Silver D, et al.: Conversion of chronic pain patients from full-opioid agonists to sublingual buprenorphine. Pain Physician. 2012; 15(3 Suppl.): ES59-ES66.
Zekry O, Gibson SB, Aggarwal A: Subanesthetic, subcutaneous ketamine infusion therapy in the treatment of chronic nonmalignant pain. J Pain Palliat Care Pharmacother. 2016; 30(2): 91-98.
Marchetti F, Coutaux A, Bellanger A, et al.: Efficacy and safety of oral ketamine for the relief of intractable chronic pain: A retrospective 5-year study of 51 patients. Eur J Pain. 2015; 19(7): 984-993.
Haroutounian S, Ratz Y, Ginosar Y, et al.: The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain: A prospective open-label study. Clin J Pain. 2016; 32(12): 1036-1043.
Levine AB, Steven DA, Parrent AG, et al.: Successful long-term nerve root stimulation for chronic neuropathic pain: A real world. Pain Physician. 2017; 20(2): 95-106.
Caraway D, Walker V, Becker L, et al.: Successful discontinuation of systemic opioids after implantation of an intrathecal drug delivery system. Neuromodulation. 2015; 18(6): 508-515, discussion 515-516. DOI: 10.1111/ner.12318.
Hooten WM, Townsend CO, Bruce BK, et al.: The effects of smoking status on opioid tapering among patients with chronic pain. Anesth Analg. 2009; 108(1): 308-315. DOI: 10.1213/ane.0b013e31818c7b99.
Huffman KL, Rush TE, Fan Y, et al.: Sustained improvements in pain, mood, function and opioid use post interdisciplinary pain rehabilitation in patients weaned from high and low dose chronic opioid therapy. Pain. 2017; 158(7): 1380-1394. DOI: 10.1097/j.pain.0000000000000907.
Goesling J, Moser SE, Lin LA, et al.: Discrepancies between perceived benefit of opioids and self-reported patient outcomes. Pain Med. 2018; 19(2): 297-306.
Smit T, Rogers AH, Garey L, et al.: Anxiety sensitivity and pain intensity independently predict opioid misuse and dependence in chronic pain patients. Psychiatry Res. 2020; 294: 113523. DOI: 10.1016/j.psychres.2020.113523.
Helmerhorst GT, Vranceanu AM, Vrahas M, et al.: Risk factors for continued opioid use one to two months after surgery for musculoskeletal trauma. J Bone Joint Surg Am. 2014; 96(6): 495-499.
Okifuji A, Hare BD: The association between chronic pain and obesity. J Pain Res. 2015; 8: 399-408.
Hays RD, Spritzer KL, Schalet BD, et al.: PROMIS®-29 v2.0 profile physical and mental health summary scores. Qual Life Res. 2018; 27(7): 1885-1891.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.