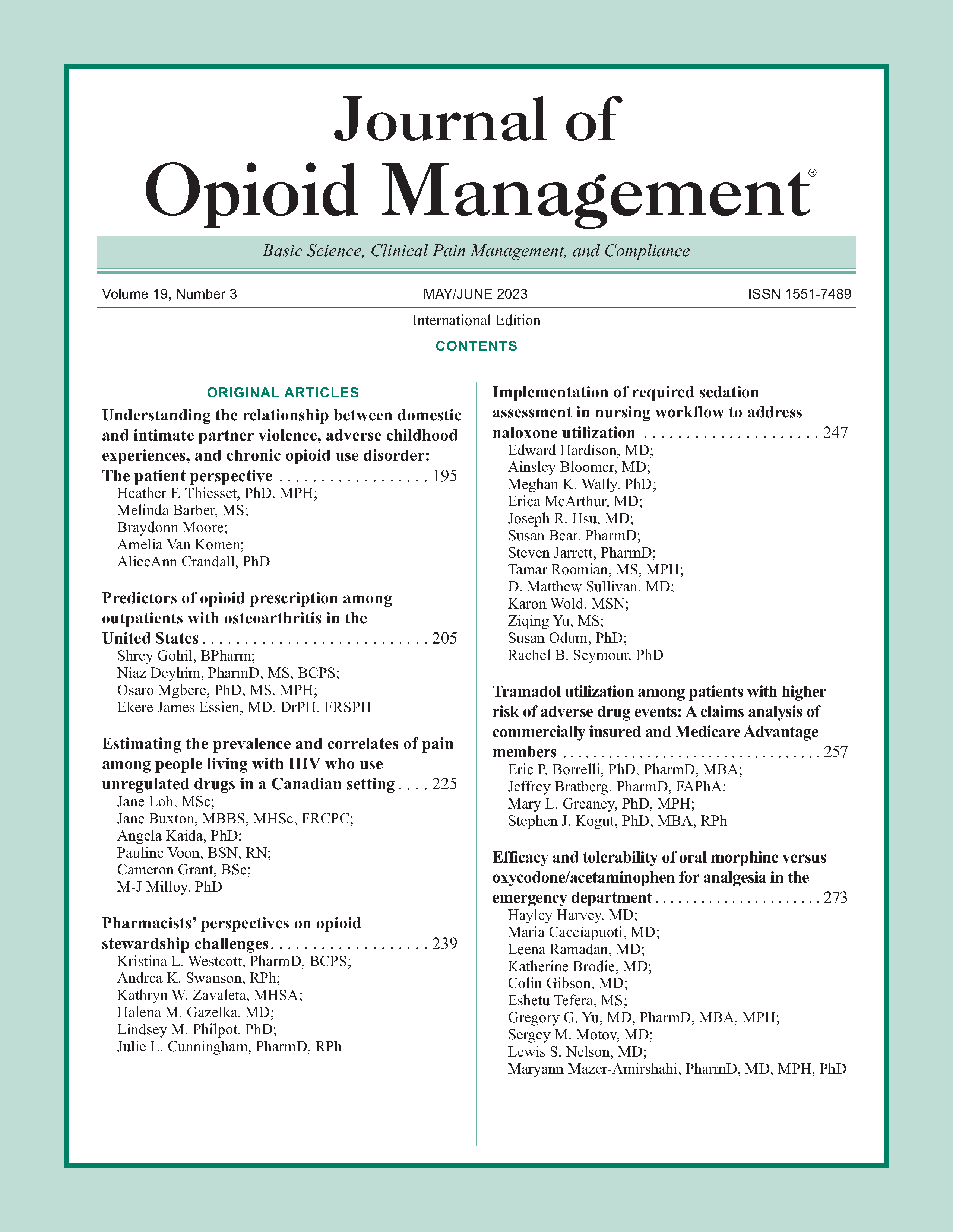
Understanding the relationship between domestic and intimate partner violence, adverse childhood experiences, and chronic opioid use disorder: The patient perspective
DOI:
https://doi.org/10.5055/jom.2023.0776Keywords:
substance use, opioid use disorder, domestic violence, intimate partner violenceAbstract
Introduction: Opioid dependence and misuse are a plague of epidemic proportions in our communities and globally. Prior trauma in childhood may contribute to opioid dependence, while one consequence of opioid misuse is increased risk for involvement as both perpetrators and victims in domestic and intimate partner violence (DV and IPV). The aims of this study were to understand the proportion of patients who identified as having an opioid use disorder (OUD), if OUD was associated with higher rates of DV and IPV as both perpetrators and victims, and whether adverse childhood experiences (ACEs) as well as demographic factors related to instability in their social life were higher among those with OUD compared to those without.
Methods: The sample consisted of 124 patients who were identified as having an OUD in their medical records based on ICD-10 codes. Each participant completed an anonymous survey about basic demographics, their alcohol, drug, and opioid intake, and their history of domestic and IPV. Descriptive statistics, univariate, and multivariate regression analyses were conducted in STATA 17.1 software.
Results: A sample of patients with an OUD diagnosis in their medical record found that 64 percent of patients acknowledged having a history of opioid addiction. Patients acknowledging OUD were more likely to not be married (divorced or single) (p < 0.01), younger than 50 years of age (p < 0.01), non-White (p < 0.01), and had higher average ACEs scores (p < 0.0X). Patients who reported OUD were also more likely to be both victims and perpetrators of DV/IPV compared to patients who denied OUD.
Discussion: OUD needs to be treated holistically to ensure that the adverse consequences of DV and IPV do not become a silent disease perpetuated on this population, their families, and society.
References
Dart RC, Surratt HL, Cicero TJ, et al.: Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015; 372(3): 241-248.
Nih NIoDA: Opioid overdose crisis. Available at https://www.drugabuse.gov/drug-topics/opioids/opioid-overdose-crisis. Accessed March 11, 2021.
Sullivan MD: Depression effects on long-term prescription opioid use, abuse, and addiction. Clin J Pain. 2018; 34(9): 878-884.
Wang S: Historical review: Opiate addiction and opioid receptors. Cell Transplant. 2019; 28(3): 233-238.
Kapitány-Fövény M, Kiss A, Farkas J, et al.: Childhood trauma, cognitive emotion regulation and motivation for behavior change among clients of opioid substitution treatment with and without past year synthetic cathinone use during therapy. Front Neurosci. 2020; 14: 37.
Moore BC, Easton CJ, McMahon TJ: Drug abuse and intimate partner violence: A comparative study of opioid-dependent fathers. Am J Orthopsychiatr. 2011; 81(2): 218-227.
Oram S, Trevillion K, Feder G, et al.: Prevalence of experiences of domestic violence among psychiatric patients: Systematic review. Br J Psychiatry. 2013; 202: 94-99.
Wentzlof CA, Boman Iv JH, Pryor C, et al.: Kicking the can down the street: Social policy, intimate partner violence, and homicide during the opioid crisis. Subst Use Misuse. 2021; 56(4): 539-545.
Breiding MJ, Smith SG, Basile KC, et al.: Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization–national intimate partner and sexual violence survey, United States, 2011. MMWR. 2014; 63(8): 1-18.
Hui V, Constantino RE: The association between life satisfaction, emotional support, and perceived health among women who experienced intimate partner violence (IPV)—2007 behavioral risk factor surveillance system. BMC Public Health. 2021; 21(1): 641.
Basile KC, Smith SG, Liu Y, et al.: Prevalence of intimate partner reproductive coercion in the United States: Racial and ethnic differences. J Interpers Violence. 2021; 36(21-22): NP12324-NP12341.
Lipsky S, Caetano R, Roy-Byrne P: Racial and ethnic disparities in police-reported intimate partner violence and risk of hospitalization among women. Women's Health Issues. 2009; 19(2): 109-118.
Gomez J, Orchowski L, Pearlman DN, et al.: Alcohol use and intimate partner violence among community college women: An exploration of protective factors. Violence Gen. 2019; 6(3): 187-195.
Neal AM, Edwards KM: Perpetrators' and victims' attributions for IPV: A critical review of the literature. Trauma Violence Abuse. 2017; 18(3): 239-267.
Sáez G, Ruiz MJ, Delclós-López G, et al.: The effect of prescription drugs and alcohol consumption on intimate partner violence victim blaming. Int J Environ Res Public Health. 2020; 17(13): 4747.
De Aquino JP, Sofuoglu M, Stefanovics E, et al.: Adverse consequences of co-occurring opioid use disorder and cannabis use disorder compared to opioid use disorder only. Am J Drug Alcohol Abuse. 2019; 45(5): 527-537.
Chermack ST, Walton MA, Fuller BE, et al.: Correlates of expressed and received violence across relationship types among men and women substance abusers. Psychol Addict Behav. 2001; 15(2): 140-151.
Dillon G, Hussain R, Loxton D, et al.: Mental and physical health and intimate partner violence against women: A review of the literature. Int J Family Med. 2013; 2013: 1-15.
Felitti VJ, Anda RF, Nordenberg D, et al.: Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. 1998; 14(4): 245-258.
Karatzias T, Shevlin M, Fyvie C, et al.: Adverse and benevolent childhood experiences in posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD): Implications for trauma-focused therapies. Eur J Psychotraumatol. 2020; 11(1): 1793599-1793599.
Merrick MT, Ford DC, Haegerich TM, et al.: Adverse childhood experiences increase risk for prescription opioid misuse. J Primary Prevent. 2020; 41(2): 139-152.
Bryant RA: Early predictors of posttraumatic stress disorder. Biol Psychiatry. 2003; 53(9): 789-795.
Hanson CL, Crandall A, Barnes MD, et al.: Family-focused public health: Supporting homes and families in policy and practice. Front Public Health. 2019; 7: 59-59.
Centers for Disease Control and Prevention: Original ACE questionnaire. 1998. Available at https://www.traumainformedcare.chcs.org/resource/original-ace-questionnaire/. Accessed September 23, 2022.
Brown KG, Capili B: CE: Opioid use disorder: Pathophysiology, assessment, and effective interventions. Am J Nurs. 2020; 120(6): 38-46.
Scorza P, Duarte CS, Hipwell AE, et al.: Research review: Intergenerational transmission of disadvantage: Epigenetics and parents' childhoods as the first exposure. J Child Psychol Psychiatr. 2019; 60(2): 119-132.
Morris AS, Hays-Grudo J, Zapata MI, et al.: Adverse and protective childhood experiences and parenting attitudes: The role of cumulative protection in understanding resilience. Adv Res Sci. 2021; 2(3): 181-192.
Quinn K, Boone L, Scheidell JD, et al.: The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug Alcohol Depend. 2016; 169: 190-198.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.