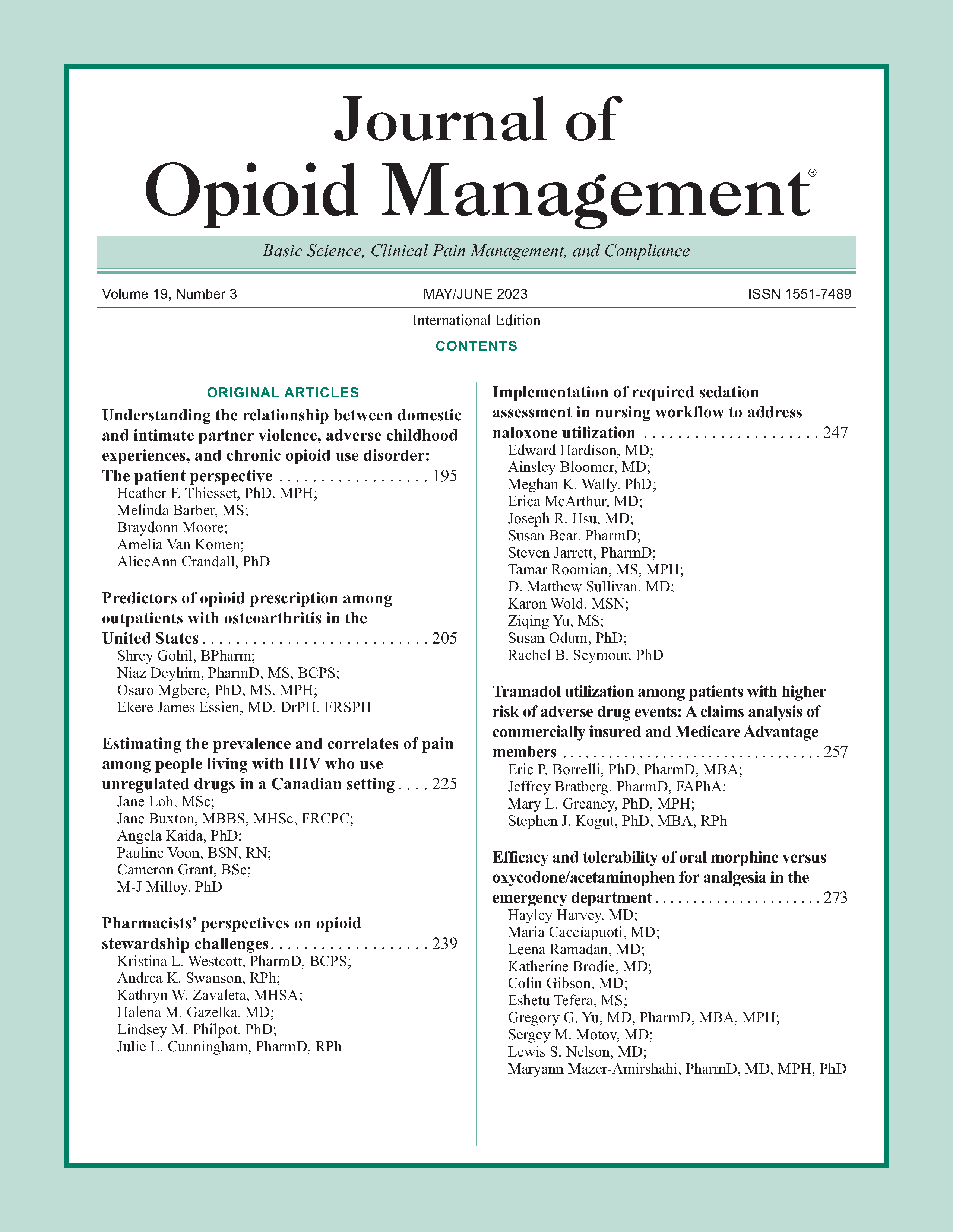
Tramadol utilization among patients with higher risk of adverse drug events: A claims analysis of commercially insured and Medicare Advantage members
DOI:
https://doi.org/10.5055/jom.2023.0781Keywords:
tramadol, contraindications, polypharmacy, benzodiazepines, serotonergic medicationsAbstract
Objective: To assess prescribing of tramadol among patients with contraindications and higher risks of adverse events in a large population of commercially insured and Medicare Advantage members.
Design: We performed a cross-sectional analysis evaluating tramadol utilization in patients with higher risk of adverse outcomes.
Setting: This study utilized 2016-2017 data from the Optum Clinformatics Data Mart.
Patients and participants: Patients with at least one tramadol prescription without a cancer or sickle cell diagnosis during the study period.
Main outcome measures: We first determined if tramadol was prescribed among patients with contraindications or risk factors for adverse outcomes. We then determined if patient demographic or clinical factors were associated with the use of tramadol in these higher-risk scenarios using multivariable logistic regression models.
Results: Among patients with at least one prescription for tramadol, 19.66 percent (99 percent CI: 19.57-19.75) concurrently received an interacting cytochrome P450 isoenzyme medication, 19.24 percent (99 percent CI: 19.15-19.33) concurrently received a serotonergic medication, and 7.93 percent (99 percent CI: 7.88-8.00) concurrently received a benzodiazepine. Additionally, 1.59 percent (99 percent CI: 1.56-1.61) of patients who received tramadol also had a seizure disorder, while 0.55 percent (99 percent CI: 0.53-0.56) of patients were under the age of 18. Overall, nearly one in three patients (31.17 percent) received tramadol in the presence of at least one of these risks (99 percent CI: 31.06-31.27).
Conclusion: Almost one in three patients prescribed tramadol had a clinically significant drug interaction or contraindication for use, suggesting that prescribers often disregard these concerns. Real-world studies are needed to better understand the likelihood of harms associated with the use of tramadol in these contexts.
References
H.J. Harkins Company Inc: Tramadol [Package Insert]. Grover Beach, CA: H.J. Harkins Company Inc, 2017.
Fuentes AV, Pineda MD, Venkata KCN: Comprehension of top 200 prescribed drugs in the US as a resource for pharmacy teaching, training and practice. Pharmacy (Basel). 2018; 6(2): 43.
ClinCalc: The top 200 drugs of 2021. Available at http://clincalc.com/DrugStats. Accessed June 1, 2021.
Drug Enforcement Administration: Schedules of controlled substances: Placement of tramadol into schedule IV. 2014. Available at https://www.deadiversion.usdoj.gov/fed_regs/rules/2014/fr0702.htm. Accessed January 14, 2020.
Gupta S, Nguyen TD, Freeman PR, et al.: Competitive Effects of Federal and State Opioid Restrictions: Evidence from the Controlled Substance Laws. Cambridge, MA: National Bureau of Economic Research, 2020. Available at https://www.nber.org/papers/w27520. Accessed August 10, 2020.
Rui P, Santo L, Ashman JJ: Trends in opioids prescribed at discharge from emergency departments among adults: United States, 2006-2017. Natl Health Stat Report. 2020; 135: 1-12.
Bigal LM, Bibeau K, Dunbar S: Tramadol prescription over a 4-year period in the USA. Curr Pain Headache Rep. 2019; 23(10): 76.
The 2019 American Geriatrics Society Beers Criteria® Update Expert Panel: American geriatrics society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019; 67(4): 674-694.
Shah A, Hayes CJ, Martin BC: Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017; 66: 265-269.
Thornton JD, Dwibedi N, Scott V, et al.: Predictors of transitioning to incident chronic opioid therapy among working-age adults in the United States. Am Health Drug Benefits. 2018; 11(1): 12-21.
Thiels CA, Habermann EB, Hooten WM, et al.: Chronic use of tramadol after acute pain episode: Cohort study. BMJ. 2019; 365: L1849.
Musich S, Wang SS, Slindee L, et al.: Characteristics associated with transition from opioid initiation to chronic opioid use among opioid-naïve older adults. Geriatr Nurs. 2019; 40(2): 190-196.
Zeng C, Dubreuil M, LaRochelle MR, et al.: Association of tramadol with all-cause mortality among patients with osteoarthritis. JAMA. 2019; 321(10): 969-982.
Xie J, Strauss VY, Martinez-Laguna D, et al.: Association of tramadol vs codeine prescription dispensation with mortality and other adverse clinical outcomes. JAMA. 2021; 326(15): 1504-1515.
Miotto K, Cho AK, Khalil MA, et al.: Trends in tramadol: Pharmacology, metabolism, and misuse. Anesth Analg. 2017; 124(1): 44-51.
Chastek B, Harley C, Kallich J, et al.: Health care costs for patients with cancer at the end of life. J Oncol Pract. 2012; 8(6): 75s-80s.
Agency for Healthcare Research and Quality: AHRQ QI™ ICD-10-CM/PCS specification version 6.0 patient safety indicators appendices; Appendix H: Cancer diagnosis codes. 2016 July. Available at https://www.qualityindicators.ahrq.gov/Downloads/Modules/PSI/V60-ICD10/TechSpecs/PSI_Appendix_H.pdf. Accessed July 14, 2020.
Surveillance, Epidemiology, and End Results Program of the National Cancer Institute: Comprehensive ICD-10-CM case-finding code list for reportable tumors. 2016. Available at https://seer.cancer.gov/tools/casefinding/case2016-icd10cm.html. Accessed July 14, 2020.
Reeves SL, Madden B, Wu M, et al.: Performance of ICD-10-CM diagnosis codes for identifying children with sickle cell anemia. Health Serv Res. 2020; 55(2): 310-317.
Yanni E, Grosse SD, Yang Q, et al.: Trends in pediatric sickle cell disease-related mortality in the United States, 1983-2002. J Pediatr. 2009; 154(4): 541-545.
Peckham AM, Evoy KE, Covvey JR, et al.: Predictors of gabapentin overuse with or without concomitant opioids in a commercially insured US population. Pharmacotherapy. 2018; 38(4): 436-443.
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain–United States, 2016. JAMA. 2016; 315(15): 1624-1645.
Swarm RA, Paice JA, Anghelescu DL, et al.: Adult cancer pain, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019; 17(8): 977-1007.
Centers for Medicare and Medicaid Services Offices of Minority Health: Opioid prescription in medicare beneficiaries: Prescription opioid policies and implications for beneficiaries with sickle cell disease. 2019. Available at https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Opioid-Prescription-in-Medicare-Beneficiaries-Report.pdf. Accessed September 20, 2020.
Volpi-Abadie J, Kaye AM, Kaye AD: Serotonin syndrome. Ochsner J. 2013; 13(4): 533-540.
Wishart DS, Knox C, Guo AC, et al.: DrugBank: A knowledgebase for drugs, drug actions and drug targets. Nucleic Acids Res. 2008; 36(Database issue): D901-D906.
Morgan JR, Schackman BR, Leff JA, et al.: Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. J Subst Abuse Treat. 2018; 85: 90-96.
Wallace L, Kadakia A: Buprenorphine transdermal system utilization. Postgrad Med. 2017; 129(1): 81-86.
Dahan A: Opioid-induced respiratory effects: New data on buprenorphine. Palliat Med. 2006; 20 (Suppl. 1): 3-8.
Daitch J, Frey ME, Silver D, et al.: Conversion of chronic pain patients from full-opioid agonists to sublingual buprenorphine. Pain Phys. 2012; 15(3 Suppl.): ES59-ES66.
Gordon AL, Snyder AF: Responsible opioid prescribing for chronic pain: Interpreting the CDC guideline, understanding new Rhode Island regulations. R I Med J. 2013; 100(10): 45-47.
Strickler GK, Zhang K, Halpin JF, et al.: Effects of mandatory prescription drug monitoring program (PDMP) use laws on prescriber registration and use and on risky prescribing. Drug Alcohol Depend. 2019; 199: 1-9.
Guy GP Jr, Zhang K, Halpin J, et al.: An examination of concurrent opioid and benzodiazepine prescribing in 9 states, 2015. Am J Prev Med. 2019; 57(5): 629-636.
Liu Y, Logan JE, Paulozzi LJ, et al.: Potential misuse and inappropriate prescription practices involving opioid analgesics. Am J Manag Care. 2013; 19(8): 648-658.
Leslie RS: Using arrays to calculate medication utilization. In SAS Global Forum 2007 April 16-19. Available at https://support.sas.com/resources/papers/proceedings/proceedings/forum2007/043-2007.pdf. Accessed November 19, 2019.
Bergen DC, Beghi E, Medina MT: Revising the ICD-10 codes for epilepsy and seizures. Epilepsia. 2012; 53 (Suppl. 2): 3-5.
Jette N, Beghi E, Hesdorffer D, et al.: ICD coding for epilepsy: Past, present, and future—A report by the international league against epilepsy task force on ICD codes in epilepsy. Epilepsia. 2015; 56(3): 348-355.
US Census Bureau: State population by characteristics: 2010-2017: Census Bureau QuickFacts. 2018. Available at https://www.census.gov/data/tables/2017/demo/popest/state-detail.html. Accessed November 15, 2019.
Elixhauser A, Steiner C, Harris DR, et al.: Comorbidity measures for use with administrative data. Med Care. 1998; 36(1): 8-27.
Quan H, Sundararajan V, Halfon P, et al.: Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11): 1130-1139.
Daly LE: Chapter 12: Confidence intervals and sample sizes. In Altman DG, Machin D, Bryant TN, et al. (eds.): Statistics with Confidence: Confidence Intervals and Statistical Guidelines. 2nd ed. United Kingdom: BMJ Books, 2011.
Sperandei S: Understanding logistic regression analysis. Biochem Med. 2014; 24(1): 12-18.
Stoltzfus JC: Logistic regression: A brief primer. Acad Emerg Med. 2011; 18(10): 1099-1104.
Greenland S: Chapter 21: Introduction to regression modeling. In Rothman KJ, Greenland S, Lash TL (eds.): Modern Epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2008.
Kleinbaum DG, Klein M: Chapter 7: Modeling strategy for assessing interaction and confounding. In Kleinbaum DG, Klein M (eds.): Logistic Regression. 2nd ed. New York: Springer, 2002: 191-226.
Hoffelt C, Gross T: A review of significant pharmacokinetic drug interactions with antidepressants and their management. Ment Health Clin. 2016; 6(1): 35-41.
Frost DA, Soric MM, Kaiser R, et al.: Efficacy of tramadol for pain management in patients receiving strong cytochrome P450 2D6 inhibitors. Pharmacotherapy. 2019; 39(6): 724-729.
Shakoor M, Ayub S, Ahad A, et al.: Transient serotonin syndrome caused by concurrent use of tramadol and selective serotonin reuptake inhibitor. Am J Case Rep. 2014; 15: 562-564.
Shahani L: Tramadol precipitating serotonin syndrome in a patient on antidepressants. J Neuropsychiatry Clin Neurosci. 2012; 24(4): E52.
Park SH, Wackernah RC, Stimmel GL: Serotonin syndrome: Is it a reason to avoid the use of tramadol with antidepressants? J Pharm Pract. 2014; 27(1): 71-78.
Kim K, Lee H, Shin JY: Explosive increase in tramadol use in Korea 2003-2013: Analysis of patient trends based on the Korea national health insurance database. J Psychoactive Drugs. 2020; 52(2): 153-161.
Birke H, Ekholm O, Sjøgren P, et al.: Tramadol use in Norway: A register-based population study. Pharmacoepidemiol Drug Saf. 2019; 28(1): 54-61.
Clarot F, Goullé JP, Vaz E, et al.: Fatal overdoses of tramadol: Is benzodiazepine a risk factor of lethality? Forensic Sci Int. 2003; 134(1): 57-61.
Hung A, Bush C, Greiner M, et al.: Risk factors and outcomes of opioid users with and without concurrent benzodiazepine use in the North Carolina Medicaid population. J Manag Care Spec. 2020; 26(2): 169-175.
McDermot D: Research brief no. 97: Pharmacy quality alliance opioid prescribing measurers in Washington state, 2014-
Washington State Office of Financial Management. 2020. Available at https://www.ofm.wa.gov/sites/default/files/public/dataresearch/researchbriefs/brief097.pdf. Accessed December 21 2021.
Borrelli EP, Morphis B, Youssef R, et al.: Concurrent utilization of prescription opioids and non-opioid controlled substances: Rhode Island prescription drug monitoring program, 2018. R I Med J. 2013; 103(8): 53-58.
Sun EC, Dixit A, Humphreys K, et al.: Association between concurrent use of prescription opioids and benzodiazepines and overdose: Retrospective analysis. BMJ. 2017; 356: J760.
US Food and Drug Administration: FDA drug safety communication: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning. 2016. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safetycommunication-fda-warns-about-serious-risks-and-deathwhen-combining-opioid-pain-or. Accessed June 30, 2020.
Caupp S, Steffan J, Shi J, et al.: Opioid drug poisonings in Ohio adolescents and young adults, 2002-2014. Clin Toxicol (Phila). 2018; 56(8): 765-772.
Shadnia S, Soltaninejad K, Heydari K, et al.: Tramadol intoxication: A review of 114 cases. Hum Exp Toxicol. 2008; 27(3): 201-205.
US Food and Drug Administration: FDA drug safety communication: FDA restricts use of prescription codeine pain and cough medicines and tramadol pain medicines in children; recommends against use in breastfeeding women. 2017. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-restricts-use-prescriptioncodeine-pain-and-cough-medicines-and. Accessed September 20, 2020.
US Food and Drug Administration: FDA drug safety communication: FDA evaluating the risks of using the pain medicine tramadol in children aged 17 and younger. 2015. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-evaluating-risks-usingpain-medicine-tramadol-children-aged-17-and. Accessed September 20, 2020.
Dusetzina SB, Higashi AS, Dorsey ER, et al.: Impact of FDA drug risk communications on health care utilization and health behaviors: A systematic review. Med Care. 2012; 50(6): 466-478.
Kesselheim AS, Sinha MS, Campbell EG, et al.: Multimodal analysis of FDA drug safety communications: Lessons from zolpidem. Drug Saf. 2019; 42(11): 1287-1295.
Major JM, Zhou EH, Ding Y, et al.: The effect of FDA drug safety communications on patterns of tiotropium dispensing: A US health plan claims database study. J Manag Care Pharm. 2018; 24(7): 700-709.
Aidarex Pharmaceuticals LLC: Tramadol [Package Insert]. Carona, CA. Aidarex Pharmaceuticals LLC, 2012.
Taghaddosinejad F, Mehrpour O, Afshari R, et al.: Factors related to seizure in tramadol poisoning and its blood concentration. J Med Toxicol. 2011; 7(3): 183-188.
Morrow RL, Dormuth CR, Paterson M, et al.: Canadian drug safety effectiveness research network (CDSERN), tramadol and the risk of seizure: Nested case-control study of US patients with employer-sponsored health benefits. BMJ Open. 2019; 9(3): e026705.
Musich S, Wang SS, Slindee LB, et al.: Concurrent use of opioids with other central nervous system-active medications among older adults. Popul Health Manag. 2020; 23(4): 286-296.
Merlin JS, Tamhane A, Starrels JL, et al.: Factors associated with prescription of opioids and co-prescription of sedating medications in individuals with HIV. AIDS Behav. 2016; 20(3): 687-698.
Maust DT, Lin LA, Blow FC: Benzodiazepine use and misuse among adults in the United States. Psychiatr Serv. 2019; 70(2): 97-106.
Makkar RR, Fromm BS, Steinman RT, et al.: Female gender as a risk factor for Torsades de Pointes associated with cardiovascular drugs. JAMA. 1993; 270: 2590-2597.
Bednar MM, Harrigan EP, Ruskin JN: Torsades de Pointes associated with nonantiarrhythmic drugs and observations on gender and QTc. Am J Cardiol. 2002; 89: 1316-1319.
Sauer AJ, Newton-Cheh C: Clinical and genetic determinants of torsade de pointes risk. Circulation. 2012; 125(13): 1684-1694.
Charlesworth CJ, Smit E, Lee DS, et al.: Polypharmacy among adults aged 65 years and older in the United States: 1988-2010. J Gerontol A Biol Sci Med Sci. 2015; 70(8): 989-995.
Kantor ED, Rehm CD, Haas JS, et al.: Trends in prescription drug use among adults in the United States from 1999-2012. JAMA. 2015; 314(17): 1818-1831.
Centers for Medicare and Medicaid Services: Concurrent use of opioids and benzodiazepines in a medicare part D population. 2016. Available at https://www.cms.gov/Medicare/Prescription-DrugCoverage/PrescriptionDrugCovContra/Downloads/Concurrent-Use-of-Opioidsand-Benzodiazepinesin-a-Medicare-Part-D-Population-CY-2015.pdf. Accessed June 13, 2020.
Morden NE, Munson JC, Colla CH, et al.: Prescription opioid use among disabled medicare beneficiaries: Intensity, trends, and regional variation. Med Care. 2014; 52(9): 852-859.
Horsky J, Drucker EA, Ramelson HZ: Accuracy and completeness of clinical coding using ICD-10 for ambulatory visits. AMIA Annu Symp Proc. 2017; 2017: 912-920.
Prescription Drug Monitoring Program Training and Technical Assistance Center: Prescription drug monitoring program: Mandatory enrollment and use of PDMPs. 2020. Available at https://www.pdmpassist.org/pdf/TAG_Mandatory_Enrollment_Use_20200710.pdf. Accessed December 21, 2021.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.