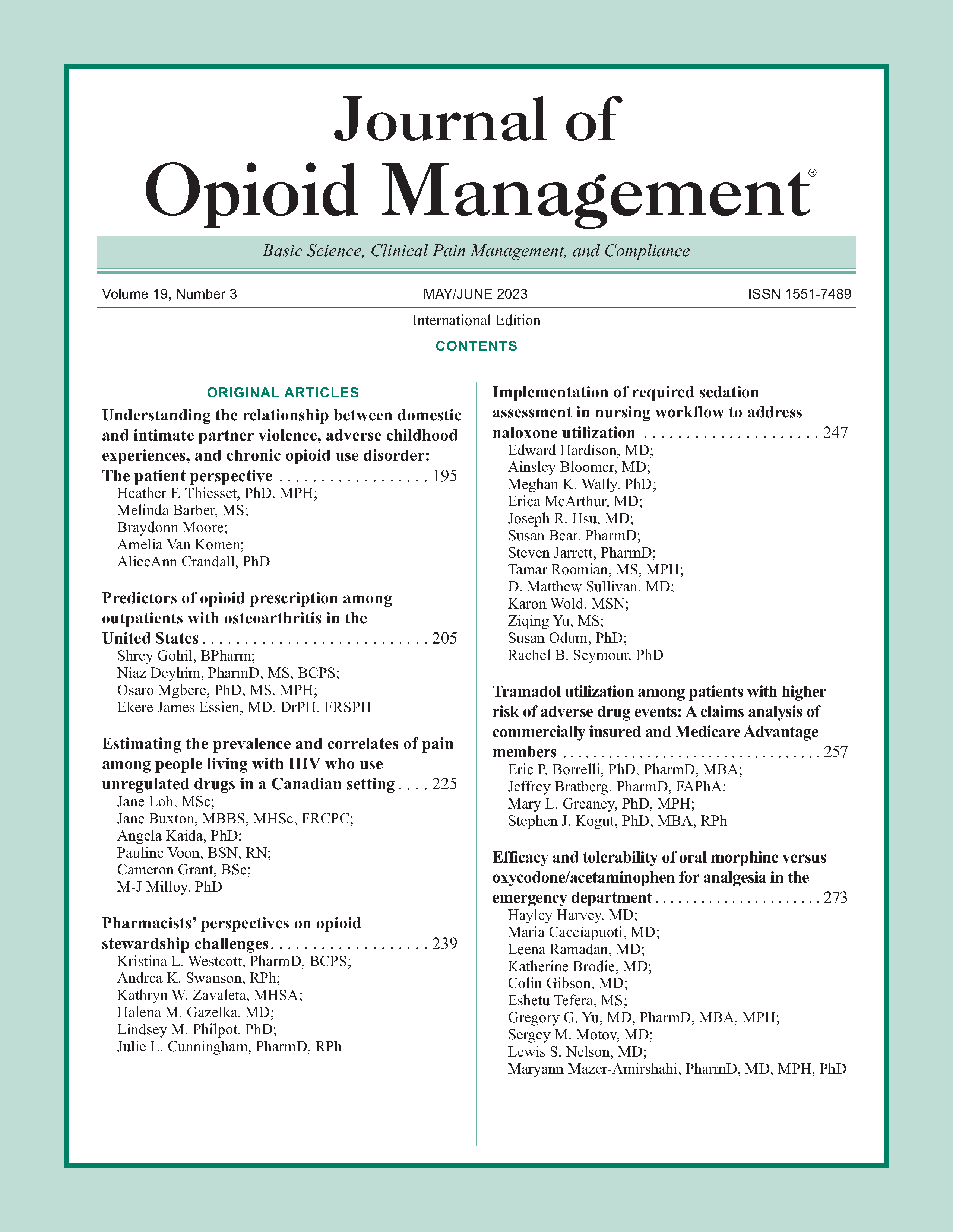
Efficacy and tolerability of oral morphine versus oxycodone/acetaminophen for analgesia in the emergency department
DOI:
https://doi.org/10.5055/jom.2023.0782Keywords:
morphine, oxycodone, opioidAbstract
Objective: Oxycodone/acetaminophen is one of the most commonly prescribed medications for pain management in the emergency department (ED) despite its high abuse liability. Our objective was to determine whether oral immediate-release morphine is as effective and well tolerated as oral oxycodone/acetaminophen for pain relief in stable ED patients.
Design: This is a prospective comparative study in which stable adult patients with acute painful conditions who had either oral morphine (15 or 30 mg) or oxycodone/ acetaminophen (5/325 mg or 10/650 mg) ordered for them at the discretion of a triage physician were recruited.
Setting: This study took place in an urban, academic ED from 2016 to 2019.
Participants: Seventy-three percent of the subjects were between the ages of 18 and 59, 57 percent were female, and 85 percent were African American. Most presented with abdominal, extremity, or back pain. Patient characteristics were similar between treatment groups.
Interventions: Of the 364 enrolled patients, 182 were given oral morphine and 182 were given oxycodone/acetaminophen at the discretion of the triage provider. They were asked to rate their pain score prior to receiving analgesia and at 60 and 90 minutes after administration.
Main outcome measures: We examined pain scores, adverse effects, overall satisfaction, willingness to accept the same treatment again, and the need for additional analgesia.
Results: There was no difference in satisfaction reported by patients who received morphine versus oxycodone/acetaminophen: 15.9 percent vs 16.5 percent were very satisfied, 31.9 percent vs 26.4 percent were somewhat satisfied, and 23.6 percent vs 22.5 percent were not satisfied, p = 0.56. Secondary outcomes also showed no significant difference: net change in pain score –2 vs –2 at 60 and 90 minutes, p = 0.91 and p = 0.72, respectively; adverse effects 20.9 percent vs 19.2 percent, p = 0.69; need for further analgesia 9.3 percent vs 7.1 percent, p = 0.44; willingness to accept analgesic again 73.1 percent vs 78.6 percent, p = 0.22.
Conclusions: Oral morphine is a feasible alternative to oxycodone/acetaminophen for analgesia in the ED.
References
CDC: Wide-Ranging Online Data for Epidemiologic Research (WONDER). Atlanta, GA: CDC, National Center for Health Statistics, 2021. Available at https://www.cdc.gov/drugoverdose/epidemic/index.html. Accessed June 6, 2021.
Wightman R, Perrone J, Portelli I, et al.: Likeability and abuse liability of commonly prescribed opioids. J Med Toxicol. 2012; 8(4): 335-340.
Kibaly C, Alderete JA, Liu SH, et al.: Oxycodone in the opioid epidemic: High ‘liking’, ‘wanting’, and abuse liability. Cell Mol Neurobiol. 2021; 41(5): 899-926.
Connors NJ, Mazer-Amirshahi M, Motov S, et al.: Relative addictive potential of opioid analgesic agents. Pain Manag. 2021; 11(2): 201-215.
Mazer-Amirshahi M, Mullins PM, Rasooly I, et al.: Rising opioid prescribing in adult US emergency department visits: 2001-2010. Acad Emerg Med. 2014; 21(3): 236-243.
Cordell WH, Keene KK, Giles BK, et al.: The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002; 20: 165-169.
Volkow ND, McLellan TA, Cotto JH, et al.: Characteristics of opioid prescriptions in 2009. JAMA. 2011; 305(13): 1299-1301.
Butler MM, Ancona RM, Beauchamp GA, et al.: Emergency department prescription opioids as an initial exposure preceding addiction. Ann Emerg Med. 2016; 68(2): 202-208.
Lyapustina T, Castillo R, Omaki E, et al.: The contribution of the emergency department to opioid pain reliever misuse and diversion: A critical review. Pain Pract. 2017; 17(8): 1097-1104.
Barnett ML, Olenski AR, Jena AB: Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. 2017; 376: 663-673.
Hintze J: PASS 12. NCSS, LLC. Kaysville, Utah, USA, 2013. Available at www.ncss.com. Accessed March 19, 2020.
Cisewski DH, Motov SM: Essential pharmacologic options for acute pain management in the emergency setting. Turk J Emerg Med. 2019; 19(1): 1-11.
Abdolrazaghnejad A, Banaie M, Tavakoli N, et al.: Pain management in the emergency department: A review article on options and methods. Adv J Emerg Med. 2018; 2(4): e45.
Cicero TJ, Ellis MS, Paradis A, et al.: Determinants of fentanyl and other potent μ opioid agonist misuse in opioid-dependent individuals. Pharmacoepidem Drug Safe. 2010; 19(10): 1057-1063.
Dasgupta N, Freifeld C, Brownstein JS, et al.: Crowdsourcing black market prices for prescription opioids. J Med Internet Res. 2013; 15(8): e178.
Manchikanti L, Fellows B, Ailinani H, et al.: Therapeutic use, abuse, and nonmedical use of opioids: A ten-year perspective. Pain Phys. 2010; 13(5): 401-435.
Davis WR, Johnson BD: Prescription opioid use, misuse, and diversion among street drug users in New York City. Drug Alcohol Depend. 2008; 92(11-3): 267-276.
Stoops WW, Hatton KW, Lofwall MR, et al.: Intravenous oxycodone, hydrocodone, and morphine in recreational opioid users: Abuse potential and relative potencies. Psychopharmacology (Berl.). 2010; 212(2): 193-203.
Guo KK, Deng CQ, Lu GJ, et al.: Comparison of analgesic effect of oxycodone and morphine on patients with moderate and advanced cancer pain: A meta-analysis. BMC Anesthesiol. 2018; 18(1): 132.
Wang YM, Liu ZW, Liu JL, et al.: Efficacy and tolerability of oxycodone in moderate-severe cancer-related pain: A metaanalysis of randomized controlled trials. Exp Ther Med. 2012; 4(2): 249-254. DOI: 10.3892/etm.2012.571.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.