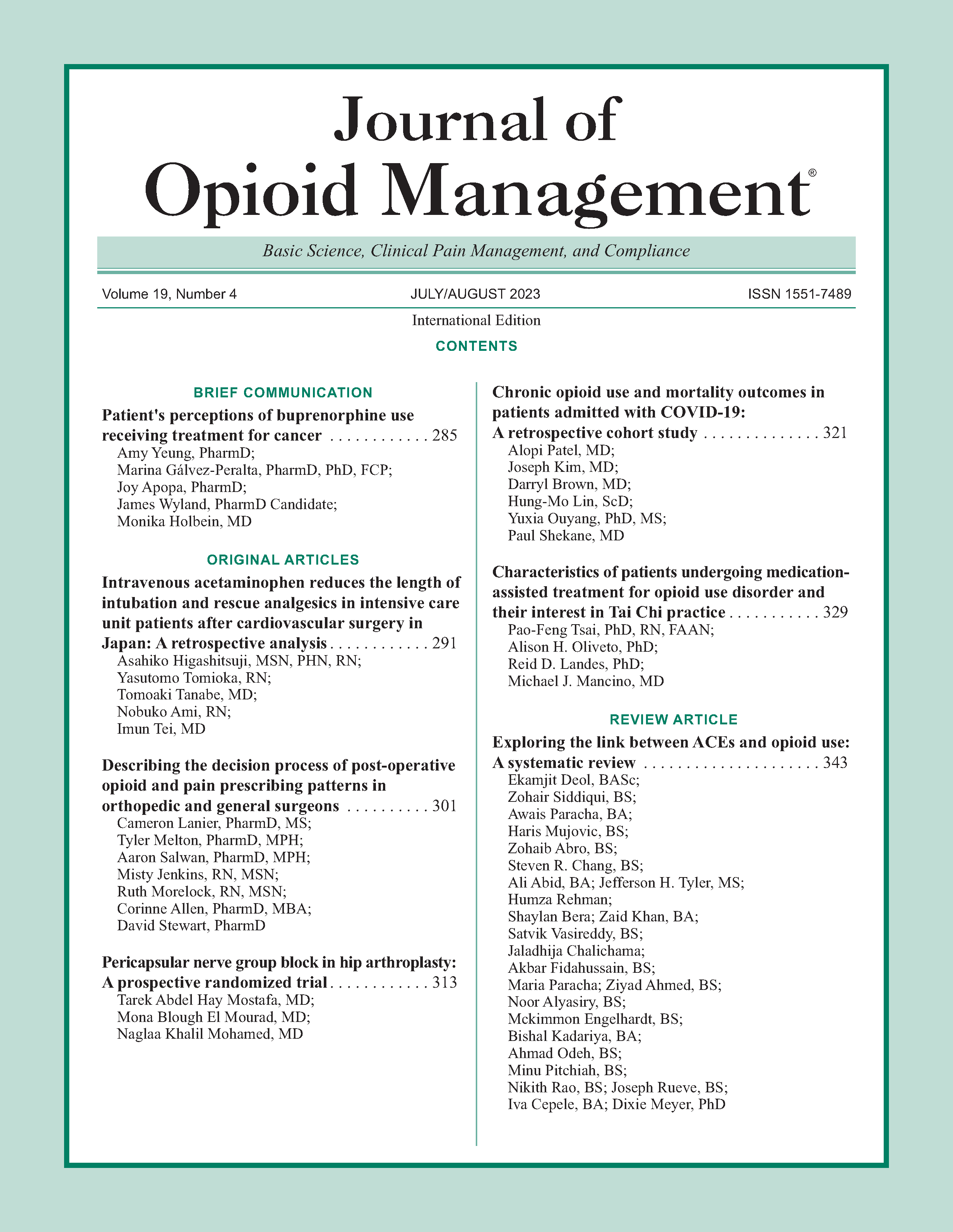
Patient's perceptions of buprenorphine use receiving treatment for cancer
DOI:
https://doi.org/10.5055/jom.2023.0785Keywords:
buprenorphine, cancer, palliative, stigma, addictionAbstract
Objective: To assess knowledge and attitudes toward opioids and buprenorphine (BUP) of patients with cancer.
Design: Single-center, single-intervention telephone survey of patients under palliative care at the cancer center.
Outcomes: Forty percent of the participants recognized the word “buprenorphine,” and 28 percent recognized BUP indication for addiction treatment. Four percent addressed potential BUP misuse. None recognized BUP indication for pain. Seventy-one percent were not worried about addiction or dependency while using opioids to treat their cancer-related-pain, and 73 percent were not worried about being stigmatized in the healthcare setting about their pain regimens. Patients on opioids for less than 3 months were most strongly correlated with the fear of addiction and stigma.
Conclusion: This study identifies patients’ knowledge gap regarding BUP products for pain, which gives professionals the opportunity to provide education. This study identified that patients are most worried early on about addiction and stigma when using opioids.
References
Dalal S, Bruera E: Pain management for patients with advanced cancer in the opioid epidemic era. Am Soc Clin Oncol Educ Book. 2019; 39: 24-35. DOI: 10.1200/EDBK_100020.
Kumar R, Viswanath O, Saadabadi A: Buprenorphine. In StatPearls. Treasure Island, FL: StatPearls Publishing, 2021. Available at https://www.ncbi.nlm.nih.gov/books/NBK459126/. Accessed November 21, 2022.
Harris PA, Taylor R, Thielke R, et al.: Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42(2): 377-381.
Harris PA, Taylor R, Minor B, et al.: REDCap consortium, the REDCap consortium: Building an international community of software partners. J Biomed Inform. 2019; 95: 103208. DOI: 10.1016/j.jbi.2019.103208.
Bulls HW, Hoogland AI, Craig D, et al.: Cancer and opioids: Patient experiences with stigma (COPES)—A pilot study. J Pain Symp Manag. 2019; 57(4): 816-819.
Schenker Y, Hamm M, Bulls HW, et al.: This is a different patient population: Opioid prescribing challenges for patients with cancer-related pain. JCO Oncol Pract. 2021; 17(7): e1030-e1037.
McCarthy M: Opioid prescribing rates in US vary widely between states. CDC reports. 2014.
Roose R, Fuentes L, Cheema M: Messages about methadone and buprenorphine in reality television: A content analysis of celebrity rehab with Dr. Drew. Subst Use Misuse. 2012; 47(10): 1117-1124. DOI: 10.3109/10826084.2012.680172.
Whelan PJ, Remsk K: Buprenorphine vs methadone treatment: A review of evidence in both developed and developing worlds. J Neurosci Rural Pract. 2012; 3(1): 45-50. DOI: 10.4103/0976-3147.91934.
Degnan M, Mousa SA: A narrative review of buprenorphine in adult cancer pain. Expert Rev Clin Pharmacol. 2020; 13(10): 1159-1167.
Louie DL, Assefa MT, McGovern MP: Attitudes of primary care physicians toward prescribing buprenorphine: A narrative review. BMC Fam Pract. 2019; 20(1): 1-8.
Van Zee A: The promotion and marketing of oxycontin: Commercial triumph, public health tragedy. AJPH. 2009; 99(2): 21-227.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.