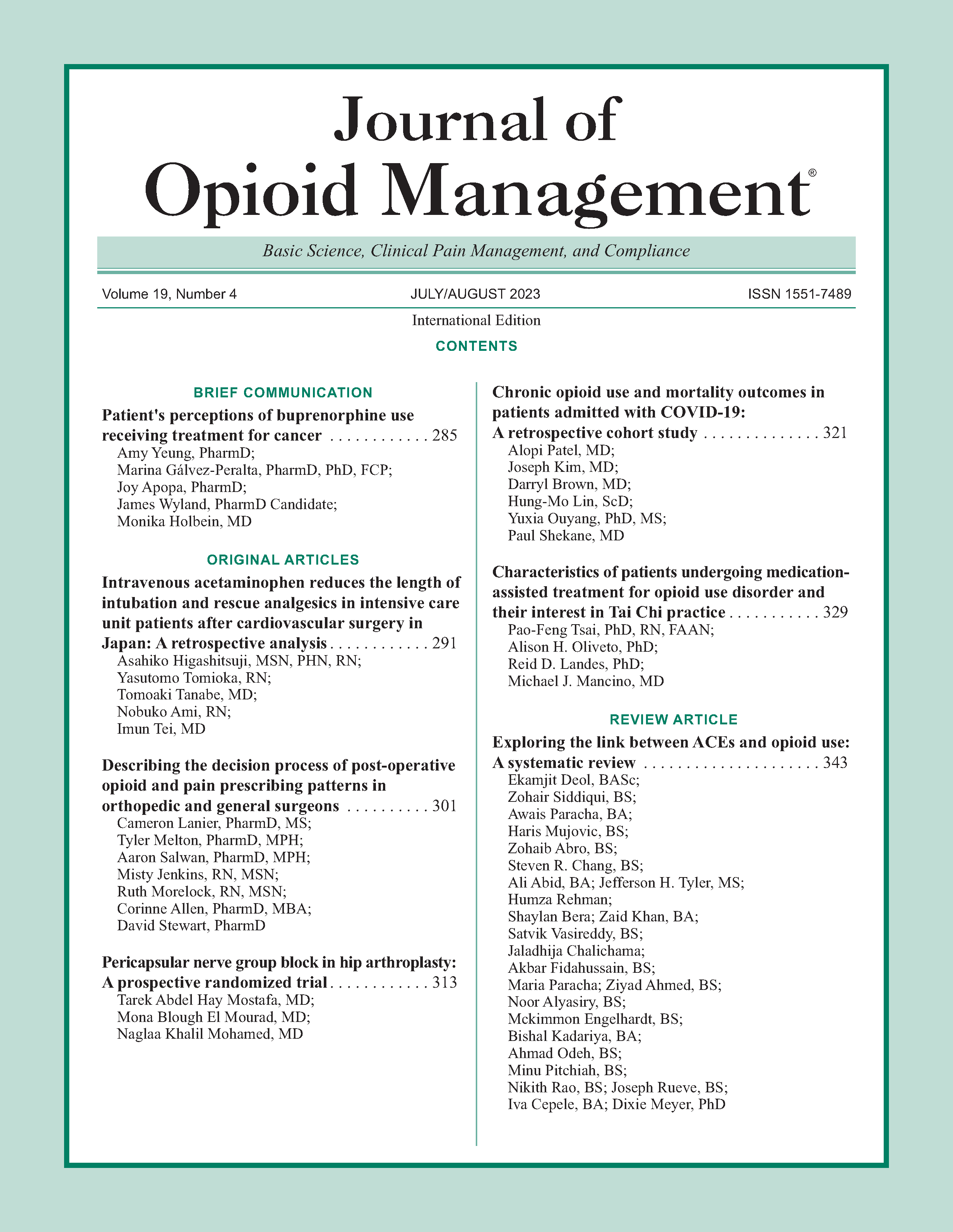
Pericapsular nerve group block in hip arthroplasty: A prospective randomized trial
DOI:
https://doi.org/10.5055/jom.2023.0788Keywords:
analgesics, opioid, bupivacaine, arthroplasty, replacement, hip, pain post-operative, nerve block, ultrasonography, morphine, analgesiaAbstract
Objectives: This study aimed to evaluate the analgesic effect of the ultrasound-guided pericapsular nerve group (PENG) block in hip arthroplasty (HA) surgery.
Design: A prospective double-blinded, randomized study.
Setting: Tertiary institutional clinical care.
Participants: Fifty patients, more than 50 years old of both genders, were chosen according to the American Society of Anesthesiologists classification, with physical status I–III, and scheduled for unilateral HA surgeries.
Interventions: Patients were randomized to receive either a sham PENG block with 20 mL of normal saline (control group) or a PENG block with 20 mL of bupivacaine 0.25 percent (PENG group).
Main outcome measures: From the onset of the first request for rescue opioid analgesia, preoperative pain scores before and after block (at rest and with a raised straight leg), the incidence of quadriceps weakness after the block, intraoperative fentanyl consumption, post-operative pain scores, and morphine consumption, besides the presence and frequency of adverse events, were recorded.
Results: The patients undergoing PENG block with bupivacaine had prolonged durations before the first analgesic request, lower perioperative pain scores, less intraoperative rescue fentanyl, and less post-operative morphine consumption than the control group, with nonsignificant motor weakness after the block and similar adverse events.
Conclusions: The PENG block provided effective perioperative analgesia for HA with prolonged duration of analgesia, nonsignificant motor effects, reduced perioperative opioids consumption, and no major side effects.
References
Brauer CA, Coca-Perraillon M, Cutler DM, et al.: Incidence and mortality of hip fractures in the United States. JAMA. 2009; 302(14): 1573-1579.
Lystad RP, Cameron CM, Mitchell RJ: Mortality risk among older Australians hospitalised with hip fracture: A population-based matched cohort study. Arch Osteoporos. 2017; 12(1): 1-8.
Hockett MM, Hembrador S, Lee A: Continuous quadratus lumborum block for post-operative pain in total hip arthroplasty: A case report. A&A Practice. 2016; 7(6): 129-131.
Yang Y, Zhao X, Dong T, et al.: Risk factors for post-operative delirium following hip fracture repair in elderly patients: A systematic review and meta-analysis. Aging Clin Exp Res. 2017; 29(2): 115-126.
Abdulla A, Adams N, Bone M, et al.: Guidance on the management of pain in older people. Age Ageing. 2013; 42: I1-57.
Girón-Arango L, Peng PW, Chin KJ, et al.: Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018; 43(8): 859-863.
Indelli PF, Grant SA, Nielsen K, et al.: Regional anesthesia in hip surgery. Clin Orthop Relat Res. 2005; 441: 250-255.
Yu HC, Moser JJ, Chu AY, et al.: Inadvertent quadriceps weakness following the pericapsular nerve group (PENG) block. Reg Anesth Pain Med. 2019; 44(5): 611-613.
Morrison SR, Magaziner J, McLaughlin MA, et al.: The impact of post-operative pain on outcomes following hip fracture. Pain. 2003; 103(3): 303-311.
Short AJ, Barnett JJG, Gofeld M, et al.: Anatomic study of innervation of the anterior hip capsule: Implication for image-guided intervention. Reg Anesth Pain Med. 2018; 43(2): 186-192.
Gerhardt M, Johnson K, Atkinson R, et al.: Characterisation and classification of the neural anatomy in the human hip joint. Hip Int. 2012; 22(1): 75-81.
Mysore K, Sancheti SA, Howells SR, et al.: Post-operative analgesia with pericapsular nerve group (PENG) block for primary total hip arthroplasty: A retrospective study. Can J Anesth/J Can Anesth. 2020; 67(11): 1673-1674.
Remily EA, Hochstein SR, Wilkie WA, et al.: The pericapsular nerve group block: A step towards outpatient total hip arthroplasty? Hip Int. 2020; 1120700020978211.
Shankar K, Rangalakshmi S, Ashwin AB, et al.: Comparative study of ultrasound guided PENG [pericapsular nerve group] block and FIB [Fascia Iliaca block] for positioning and postoperative analgesia prior to spinal anaesthesia for hip surgeries: Prospective randomized comparative clinical study. Indian J Anesth Analg. 2020; 7(3): 798-803.
Ueshima H, Otake H: Clinical experiences of pericapsular nerve group (PENG) block for hip surgeries. J Clin Anesh. 2018; 51: 60-61.
Alrefaey AK, Abouelela MA: Pericapsular nerve group block for analgesia of positioning pain during spinal anesthesia in hip fracture patients, a randomized controlled study. Egypt J Anaesth. 2020; 36(1): 234-239.
Roy R, Agarwal G, Pradhan C, et al.: Total post-operative analgesia for hip surgeries, PENG block with LFCN block. Reg Anesth Pain Med. 2019; 44: 684. DOI: 10.1136/rapm-2019-100454.
Girón-Arango L, Tran J, Peng PW: Reply to Aydin et al.: A novel indication of pericapsular nerve group block: Surgical anesthesia for vein ligation and stripping. J Cardiothorac Vasc Anesth. 2020; 34(3): 845-846.
Abdallah FW, Halpern SH, Aoyama K, et al.: Will the real benefits of single-shot interscalene block please stand up? A systematic review and meta-analysis. Anesth Analg. 2015; 120(5): 1114-1129.
Santos O, Pereira R, Cabral T, et al.: Is continuous PENG block the new 3-in-1? J Anesth Clin Res. 2019; 10(898): 2.
Nielsen ND, Bendtsen TF: Motor-sparing regional analgesia for hip-derived pain. Reg Anesth Pain Med. 2019; 44(3): 415-415.
Dangle J, Kukreja P, Kalagara H: Review of current practices of peripheral nerve blocks for hip fracture and surgery. Curr Anesthesiol Rep. 2020; 10: 259-266.
Morrison C, Brown B, Lin DY, et al.: Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: A scoping review. Reg Anesth Pain Med. 2021; 46(2): 169-175.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.