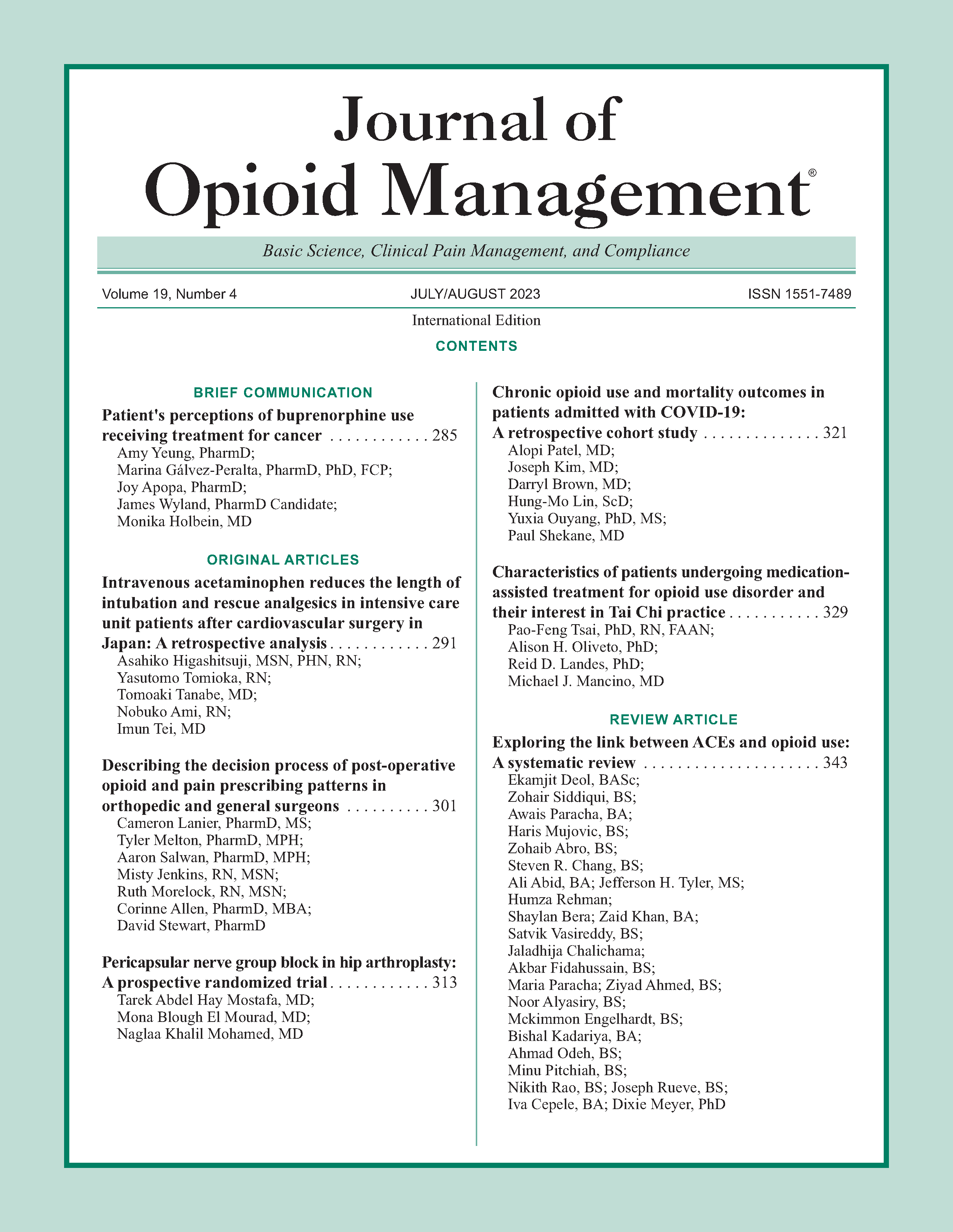
Chronic opioid use and mortality outcomes in patients admitted with COVID-19: A retrospective cohort study
DOI:
https://doi.org/10.5055/jom.2023.0789Keywords:
COVID-19, opioids, immunosuppression, chronic painAbstract
Background: We hypothesized that chronic opioid users would likely have worse outcomes with COVID-19 infection.
Methods: A retrospective review of electronic medical records was conducted for all COVID-19 patients admitted in two large academic hospitals in New York City from March 1, 2020 to June 30, 2020 during the onset of the COVID-19 pandemic. A total of 1,361 patients (1,289 opioid naïve patients, 72 with chronic opioid use) were included. A propensity score matched analysis was used to create a dataset. A logistic regression using the generalized estimating equations method was used to evaluate oxygen requirements including bilevel positive airway pressure (BiPAP), high flow nasal cannula (HFNC), and mechanical ventilation (MV). Cox models with random match pairs were fitted for time spent until hospital discharge and in-hospital mortality.
Results: The propensity score matched analysis did not demonstrate a significant difference between the chronic opioid use group vs the opioid naïve group for the use of oxygen support (p = 0.439), BiPAP (p = 0.377), HFNC (p = 0.978), or MV (p = 0.080), and length of stay (LOS) (p = 0.950). There was also no statistically significant finding for reduced need for MV (odds ratio 0.42, 95 percent CI: 0.16-1.11, p = 0.080) and lower in-hospital mortality (hazard ratio 0.75, 95 percent CI: 0.39-1.43, p = 0.378) in the chronic opioid use group; however, future larger studies will be needed.
Conclusions: Our study did not demonstrate a significant difference in outcomes in patients with COVID-19 with preadmission chronic opioid use vs opioid naïve patients in oxygen requirements, LOS, MV, or mortality. Future studies are needed to further illustrate the impact of opioids on COVID-19 outcomes.
References
Bialek S, Bowen V, Chow N, et al.: Geographic differences in COVID-19 cases, deaths, and incidence—United States, February 12–April 7, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69: 465-471.
Zhou F, Yu T, Du R, et al.: Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet (London, England). 2020; 395(10229): 1054-1062. DOI: 10.1016/S0140-6736(20)30566-3.
Barnett K, Mercer SW, Norbury M, et al.: Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet (London, England). 2012; 380(9836): 37-43. DOI: 10.1016/S0140-6736(12)60240-2.
Smith D, Wilkie R, Uthman O, et al.: Chronic pain and mortality: A systematic review. PLoS One. 2014; 9(6): e99048. DOI: 10.1371/journal.Pone.0099048.
Johannes CB, Le TK, Zhou X, et al.: The prevalence of chronic pain in United States adults: Results of an internet-based survey. J Pain. 2010; 11: 1230-1239. DOI: 10.1016/j.jpain.2010.07.002.
Centers for Disease Control and Prevention: FastStats. Therapeutic drug use. 2014. Available at http://www.cdc.gov/nchs/fastats/drug-use-therapeutic.htm. Accessed March 1, 2021.
Roy S, Wang J, Kelschenbach J, et al.: Modulation of immune function by morphine: Implications for susceptibility to infection. J NeuroImmune Pharm. 2006; 1(2006): 77-89. DOI: 10.1007/s11481-005-9009-8.
Edelman EJ, Gordon KS, Crothers K, et al.: Association of prescribed opioids with increased risk of community-acquired pneumonia among patients with and without HIV. JAMA Intern Med. 2019; 179(3): 297-304. DOI: 10.1001/jamainternmed.2018.6101.
Plein LM, Rittner HL: Opioids and the immune system—Friend or foe. Br J Pharmacol. 2018; 175(14): 2717-2725. DOI: 10.1111/bph.13750.
Bakr MA-E-M, Amr SA-ER, Mohamed SA, et al.: Comparison between the effects of intravenous morphine, tramadol, and ketorolac on stress and immune responses in patients undergoing modified radical mastectomy. Clin J Pain. 2016; 32(10): 889-897. DOI: 10.1097/AJP.0000000000000338.
Peterson PK: The opioid-cytokine connection. J Neuroimmunol. 1998; 83(1-2): 63-69. DOI: 10.1016/s0165-5728(97)00222-1.
Vallejo R: Opioid therapy and immunosuppression: A review. Am J Therap. 2004; 11(5): 354-365. DOI: 10.1097/01.mjt.0000132250.95650.85.
Wang J, Barke RA, Ma J, et al.: Opiate abuse, innate immunity, and bacterial infectious diseases. Arch Immunol Ther Exp. 2008; 56: 299-309. DOI: 10.1007/s00005-008-0035-0.
Raj CTD, Kandaswamy DK, Danduga RCSR, et al.: COVID-19: Molecular pathophysiology, genetic evolution and prospective therapeutics—A review. Arch Microbiol. 2021; 203: 2043-2015. DOI: 10.1007/s00203-021-02183-z.
Du J-Y: Effect of systemic injection of heterogenous and homogenous opioids on peripheral cellular immune response in rats with bone cancer pain: A comparative study. Exp Therap Med. 2016; 12(4): 2568-2576. DOI: 10.3892/etm.2016.3647.
Carr DJ: Exogenous and endogenous opioids as biological response modifiers. Immunopharmacology. 1995; 31(1): 59-71. DOI: 10.1016/0162-3109(95)00033-6.
Pirkle S: Chronic opioid use is associated with surgical site infection after lumbar fusion. Spine. 2020; 45(12): 837-842. DOI: 10.1097/BRS.0000000000003405.
Cismaru CA, Cismaru GL, Nabavi SF, et al.: Multiple potential targets of opioids in the treatment of acute respiratory distress syndrome from COVID-19. J Cell Mol Med. 2021; 25: 591-595. DOI: 10.1111/jcmm.15927.
El-Ashmawy NE, Lashin AA, Okasha KM, et al.: The plausible mechanisms of tramadol for treatment of COVID-19. Med Hypotheses. 2021; 146: 110468. DOI: 10.1016/j.mehy.2020.110468.
Hales CM, Martin CB, Gu Q: Prevalence of prescription pain medication use among adults: United States 2015–2018. NCHS Data Brief, no 369. Hyattsville, MD: National Center for Health Statistics, 2020.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.