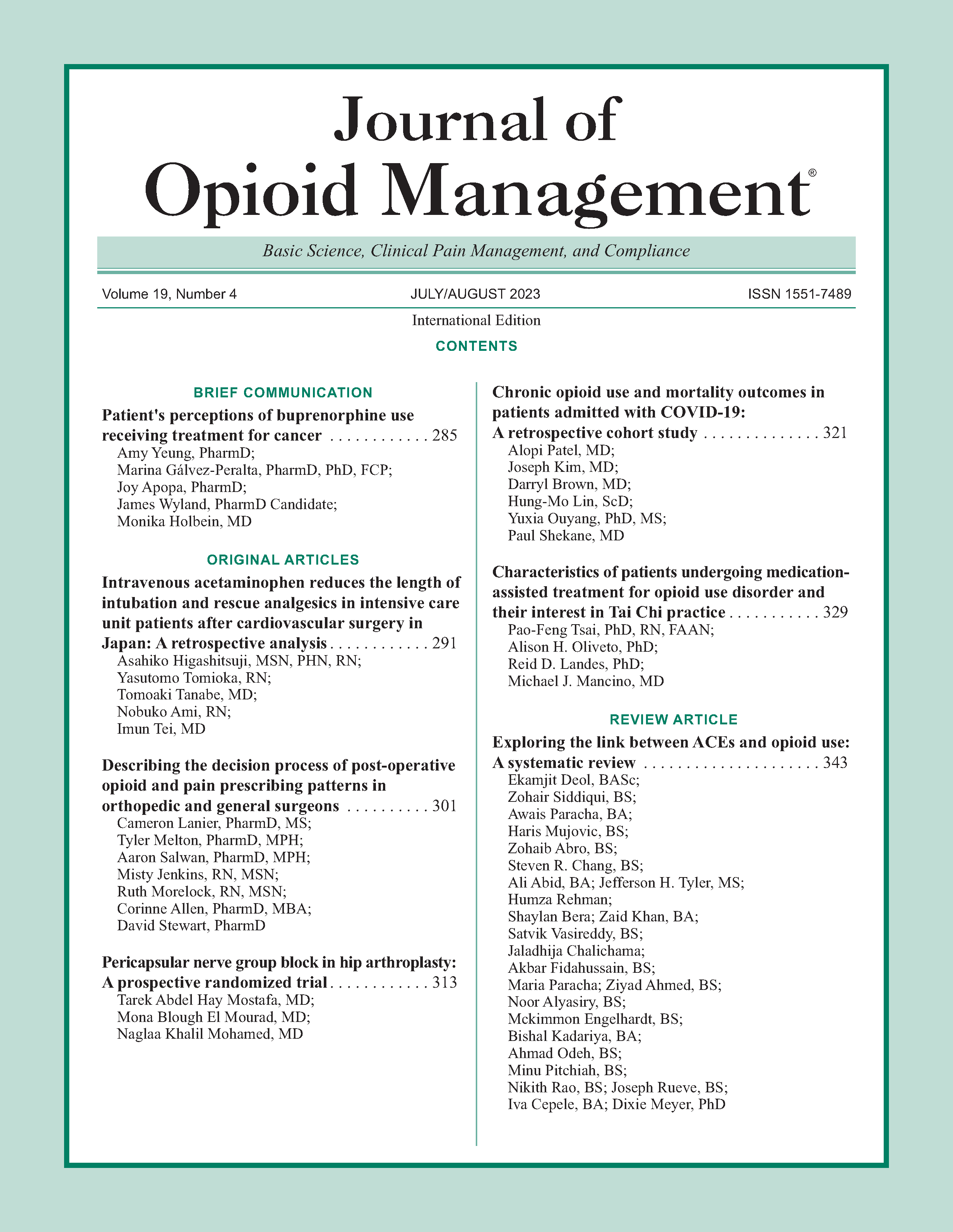
Characteristics of patients undergoing medication-assisted treatment for opioid use disorder and their interest in Tai Chi practice
DOI:
https://doi.org/10.5055/jom.2023.0790Keywords:
opioid use disorder, medication-assisted therapy, Tai Chi, pain, physical limitations, psychiatric symptomsAbstract
Objectives: (1) To explore the characteristics of patients with opioid use disorder (OUD) maintained on either methadone or buprenorphine and (2) to determine the relative acceptability of integrating Tai Chi (TC) practice into an ongoing medication- assisted treatment for opioid use disorder (MOUD) program.
Design: Survey study.
Setting: The University of Arkansas for Medical Sciences Center for Addiction Services and Treatment Program.
Patients: 97 patients receiving MOUD treatment.
Main outcomes: Drug use history, treatment status, physical limitation, mental health, pain, and whether participants were interested in using TC to improve health outcomes.
Results: At least 30.9 percent of the sample reported moderate or higher level of limitation in performing rigorous physical activities, pain intensity, and pain interference. Between 37.1 and 61.5 percent of the sample reported various psychiatric symptoms. Methadone patients reported higher levels of physical limitations, especially in rigorous activities (p = .012), climbing several flights of stairs (p = .001), and walking more than a mile (p = .011), but similar levels of pain (ps = .664-.689) and psychiatric symptoms (ps = .262-.879) relative to buprenorphine patients. At least 40.2 percent of participants expressed moderate or higher level of interest in TC for improving health outcomes, with methadone patients more interested in participating to ease mental and sleep problems (p = .005) and improve physical fitness (p = .015) compared to buprenorphine patients.
Conclusions: High prevalence of physical limitation, pain, and psychiatric comorbidities were found in OUD patients. Since patients were interested in TC to improve their health outcomes, this low-cost intervention, if proven effective, can be integrated into ongoing MOUD programs to improve health in this population.
References
Substance Abuse Center for Behavioral Health Statistics and Quality: Results from the 2020 National Survey on Drug Use and Health: Detailed tables. Substance Abuse Center for Behavioral Health Statistics and Quality. June 3, 2022. Available at https://nida.nih.gov/download/21349/medications-to-treat-opioid-use-disorder-research-report.pdf?v=99088f7584dac93ddcfa98648065bfbe. Accessed June 3, 2022.
Council of Economic Advisers: The Underestimated Cost of the Opioid Crisis, E.O.o.t.P.o.t.U. States, Editor. 2017, Executive Office of the President of the United States: Washington, DC.
Florence C, Luo F, Rice K: The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug Alcohol Depend. 2021; 218: 108350. DOI: 10.1016/j.drugalcdep.2020.108350.
Hedegaard H, Miniño AM, Warner M: Drug overdose deaths in the United States. NCHS Data Brief. 1999–2017; 2018(329): 1-8.
Saxon AJ, McCance-Katz EF: Some additional considerations regarding the American Society of Addiction Medicine National Practice guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2016; 10(3): 140-142. DOI: 10.1097/ADM.0000000000000219.
Hser YI, Saxon AJ, Huang D, et al.: Treatment retention among patients randomized to buprenorphine/naloxone compared to methadone in a multi-site trial. Addiction. 2014; 109(1): 79-87. DOI: 10.1111/add.12333.
Burns L, Gisev N, Larney S, et al.: A longitudinal comparison of retention in buprenorphine and methadone treatment for opioid dependence in New South Wales, Australia. Addiction. 2015; 110(4): 646-655. DOI: 10.1111/add.12834.
Zhu Y, Evans EA, Mooney LJ, et al.: Correlates of long-term opioid abstinence after randomization to methadone versus buprenorphine/naloxone in a multi-site trial. J Neuroimmune Pharmacol. 2018; 13(4): 488-497. DOI: 10.1007/s11481-018-9801-x.
Levine AR, Lundahl LH, Ledgerwood DM, et al.: Gender-specific predictors of retention and opioid abstinence during methadone maintenance treatment. J Subst Abuse Treat. 2015; 54: 37-43. DOI: 10.1016/j.jsat.2015.01.009.
Jones HE, Terplan M, Meyer M: Medically assisted withdrawal (detoxification): Considering the mother-infant dyad. J Addict Med. 2017; 11(2): 90-92. DOI: 10.1097/ADM.0000000000000289.
Rosenblum A, Joseph H, Fong C, et al.: Prevalence and characteristics of chronic pain among chemically dependent patients in methadone maintenance and residential treatment facilities. JAMA. 2003; 289(18): 2370-2378. DOI: 10.1001/jama.289.18.2370.
Jamison RN, Kauffman J, Katz NP: Characteristics of methadone maintenance patients with chronic pain. J Pain Symptom Manage. 2000; 19(1): 53-62.
Peles E, Schreiber S, Gordon J, et al.: Significantly higher methadone dose for methadone maintenance treatment (MMT) patients with chronic pain. Pain. 2005; 113(3): 340-346. DOI: 10.1016/j.pain.2004.11.011.
Hser YI, Mooney LJ, Saxon AJ, et al.: Chronic pain among patients with opioid use disorder: Results from electronic health records data. J Subst Abuse Treat. 2017; 77: 26-30. DOI: 10.1016/j.jsat.2017.03.006.
Ilgen MA, Trafton JA, Humphreys K: Response to methadone maintenance treatment of opiate dependent patients with and without significant pain. Drug Alcohol Depend. 2006; 82(3): 187-193. DOI: 10.1016/j.drugalcdep.2005.09.005.
Higgins C, Smith BH, Matthews K: Substance misuse in patients who have comorbid chronic pain in a clinical population receiving methadone maintenance therapy for the treatment of opioid dependence. Drug Alcohol Depend. 2018; 193: 131-136. DOI: 10.1016/j.drugalcdep.2018.08.038.
Dennis BB, Roshanov PS, Bawor M, et al.: Usefulness of the brief pain inventory in patients with opioid addiction receiving methadone maintenance treatment. Pain Physician. 2016; 19(1): E181-E195.
Morin CM, Belleville G, Belanger L, et al.: The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011; 34(5): 601-608.
Brands B, Blake J, Sproule B, et al.: Prescription opioid abuse in patients presenting for methadone maintenance treatment. Drug Alcohol Depend. 2004; 73(2): 199-207.
Barry DT, Savant JD, Beitel M, et al.: Pain and associated substance use among opioid dependent individuals seeking office-based treatment with buprenorphine-naloxone: A needs assessment study. Am J Addict. 2013; 22(3): 212-217. DOI: 10.1111/j.1521-0391.2012.00327.x.
Rhee TG, Rosenheck RA: Association of current and past opioid use disorders with health-related quality of life and employment among US adults. Drug Alcohol Depend. 2019; 199: 122-128. DOI: 10.1016/j.drugalcdep.2019.03.004.
Roncero C, Barral C, Rodriguez-Cintas L, et al.: Psychiatric comorbidities in opioid-dependent patients undergoing a replacement therapy programme in Spain: The PROTEUS study. Psychiatry Res. 2016; 243: 174-181. DOI: 10.1016/j.psychres.2016.06.024.
Rounsaville BJ, Weissman MM, Crits-Christoph K, et al.: Diagnosis and symptoms of depression in opiate addicts. Course and relationship to treatment outcome. Arch Gen Psychiatry. 1982; 39(2): 151-156.
Stein MD, Herman DS, Bishop S, et al.: Sleep disturbances among methadone maintained patients. J Subst Abuse Treat. 2004; 26(3): 175-180. DOI: 10.1016/S0740-5472(03)00191-0.
Tsui JI, Lira MC, Cheng DM, et al.: Chronic pain, craving, and illicit opioid use among patients receiving opioid agonist therapy. Drug Alcohol Depend. 2016; 166: 26-31. DOI: 10.1016/j.drugalcdep.2016.06.024.
Griffin ML, McDermott KA, McHugh RK, et al.: Longitudinal association between pain severity and subsequent opioid use in prescription opioid dependent patients with chronic pain. Drug Alcohol Depend. 2016; 163: 216-221. DOI: 10.1016/j.drugalcdep.2016.04.023.
American Society of Addiction Medicine: The ASAM Treatment of Opioid Use Disorder Course. American Society of Addiction Medicine. Available at http://depts.washington.edu/uwconf/nwrhc2018/ASAM_Treatment_of_Opioid_Use.pdf. Accessed May 18, 2019.
Huhn AS, Sweeney MM, Brooner RK, et al.: Prefrontal cortex response to drug cues, craving, and current depressive symptoms are associated with treatment outcomes in methadone-maintained patients. Neuropsychopharmacology. 2019; 44(4): 826-833. DOI: 10.1038/s41386-018-0252-0.
Zhong N, Yuan Y, Chen H, et al.: Effects of a randomized comprehensive psychosocial intervention based on cognitive behavioral therapy theory and motivational interviewing techniques for community rehabilitation of patients with opioid use disorders in Shanghai, China. J Addict Med. 2015; 9(4): 322-330. DOI: 10.1097/ADM.0000000000000139.
Ferri M, Finlayson AJ, Wang L, et al.: Predictive factors for relapse in patients on buprenorphine maintenance. Am J Addict. 2014; 23(1): 62-67. DOI: 10.1111/j.1521-0391.2013.12074.x.
Heiwe S, Lonnquist I, Kallmen H: Potential risk factors associated with risk for drop-out and relapse during and following withdrawal of opioid prescription medication. Eur J Pain. 2011; 15(9): 966-970. DOI: 10.1016/j.ejpain.2011.03.006.
Domino KB, Hornbein TF, Polissar NL, et al.: Risk factors for relapse in health care professionals with substance use disorders. JAMA. 2005; 293(12): 1453-1460. DOI: 10.1001/jama.293.12.1453.
Staedt J, Wassmuth F, Stoppe G, et al.: Effects of chronic treatment with methadone and naltrexone on sleep in addicts. Eur Arch Psychiatry Clin Nuerosci. 1996; 246(6): 305-309.
Clark RE, Baxter JD, Aweh G, et al.: Risk factors for relapse and higher costs among Medicaid members with opioid dependence or abuse: Opioid agonists, comorbidities, and treatment history. J Subst Abuse Treat. 2015; 57: 75-80. DOI: 10.1016/j.jsat.2015.05.001.
Carroll KM, Nich C, Frankforter TL, et al.: Accounting for the uncounted: Physical and affective distress in individuals dropping out of oral naltrexone treatment for opioid use disorder. Drug Alcohol Depend. 2018; 192: 264-270. DOI: 10.1016/j.drugalcdep.2018.08.019.
Benningfield MM, Dietrich MS, Jones HE, et al.: Opioid dependence during pregnancy: Relationships of anxiety and depression symptoms to treatment outcomes. Addiction. 2012; 107 Suppl. 1: 74-82. DOI: 10.1111/j.1360-0443.2012.04041.x.
National Center for Complementary and Integrative Health: NCCIH Strategic Plan FY 2021–2025. U.S. Department of Health & Human Services, National Institutes of Health, National Center for Complementary and Integrative Health. 2022. Available at https://www.nccih.nih.gov/about/nccih-strategic-plan-2021-2025. Accessed June 3, 2022.
Morris L, Stander J, Ebrahim W, et al.: Effect of exercise versus cognitive behavioural therapy or no intervention on anxiety, depression, fitness and quality of life in adults with previous methamphetamine dependency: A systematic review. Addict Sci Clin Pract. 2018; 13(1): 4. DOI: 10.1186/s13722-018-0106-4.
Purani H, Friedrichsen S, Allen AM: Sleep quality in cigarette smokers: Associations with smoking-related outcomes and exercise. Addict Behav. 2019; 90: 71-76. DOI: 10.1016/j.addbeh.2018.10.023.
Jia D, Zhou J, Xu Y: Effectiveness of traditional Chinese Health-Promoting exercise as an adjunct therapy for drug use disorders: A systematic review and meta-analysis. J Integr Complement Med. 2022; 28(4): 294-308. DOI: 10.1089/jicm.2021.0285.
Dowla R, Sinmaz H, Mavros Y, et al.: The effectiveness of exercise as an adjunct intervention to improve quality of life and mood in substance use disorder: A systematic review. Subst Use Misuse. 2022; 57(6): 911-928. DOI: 10.1080/10826084.2022.2052098.
Zhu D, Dai G, Xu D, et al.: Long-term effects of tai chi intervention on sleep and mental health of female individuals with dependence on amphetamine-type stimulants. Front Psychol. 2018; 9(1476). DOI: 10.3389/fpsyg.2018.01476.
Li DX, Zhuang XY, Zhang YP, et al.: Effects of tai chi on the protracted abstinence syndrome: A time trial analysis. Am J Chin Med. 2013; 41(1): 43-57. DOI: 10.1142/S0192415X13500043.
Zhuang SM, An SH, Zhao Y: Yoga effects on mood and quality of life in Chinese women undergoing heroin detoxification: A randomized controlled trial. Nurs Res. 2013; 62(4): 260-268. DOI: 10.1097/NNR.0b013e318292379b.
Lander L, Chiasson-Downs K, Andrew M, et al.: Yoga as an adjunctive intervention to medication-assisted treatment with buprenorphine+naloxone. J Addict Res Ther. 2017; 8(1): 354. DOI: 10.4172/2155-6105.1000354.
Tsai PF, Chang JY, Beck C, et al.: A supplemental report to a randomized cluster trial of a 20-week sun-style tai chi for osteoarthritic knee pain in elders with cognitive impairment. Complement Ther Med. 2015; 23(4): 570-576. DOI: 10.1016/j.ctim.2015.06.001.
Tsai PF, Chang JY, Beck C, et al.: A pilot cluster-randomized trial of a 20-week tai chi program in elders with cognitive impairment and osteoarthritic knee: Effects on pain and other health outcomes. J Pain Symp Manage. 2013; 45(4): 660-669. DOI: 10.1016/j.jpainsymman.2012.04.009.
Hall AM, Maher CG, Lam P, et al.: Tai Chi exercise for treatment of pain and disability in people with persistent low back pain: A randomized controlled trial. Arthritis Care Res. 2011; 63(11): 1576-1583. DOI: 10.1002/acr.20594.
Brismee JM, Paige RL, Chyu MC, et al.: Group and homebased tai chi in elderly subjects with knee osteoarthritis: A randomized controlled trial. Clin Rehabil. 2007; 21(2): 99-111.
Song R, Lee EO, Lam P, et al.: Effects of a sun-style tai chi exercise on arthritic symptoms, motivation and the performance of health behaviors in women with osteoarthritis. Taehan Kanho Hakhoe Chi. 2007; 37(2): 249-256.
Fransen M, Nairn L, Winstanley J, et al.: Physical activity for osteoarthritis management: A randomized controlled clinical trial evaluating hydrotherapy or tai chi classes. Arthritis Rheum. 2007; 57(3): 407-414.
Wang C, Schmid CH, Hibberd PL, et al.: Chi is effective in treating knee osteoarthritis: A randomized controlled trial. Arthritis Rheum. 2009; 61(11): 1545-1553.
Manubay J, Davidson J, Vosburg S, et al.: Sex differences among opioid-abusing patients with chronic pain in a clinical trial. J Addict Med. 2015; 9(1): 46-52. DOI: 10.1097/ADM.0000000000000086.
Weiss RD, Potter JS, Griffin ML, et al.: Reasons for opioid use among patients with dependence on prescription opioids: The role of chronic pain. J Subst Abuse Treat. 2014; 47(2): 140-145. DOI: 10.1016/j.jsat.2014.03.004.
Beitel M, Stults-Kolehmainen M, Cutter CJ, et al.: Physical activity, psychiatric distress, and interest in exercise group participation among individuals seeking methadone maintenance treatment with and without chronic pain. Am J Addict. 2016; 25(2): 125-131. DOI: 10.1111/ajad.12336.
Ware JE Jr, Sherbourne CD: The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992; 30(6): 473-483.
Reckitt Benckiser Pharmaceuticals Inc., Subutex (buprenorphine): Highlights of prescribing information. 2011, Reckitt Benckiser Pharmaceuticals Inc.
Hikma Pharmaceuticals USA Inc.: Methadone hydrochloride solution. Highlights of prescribing information. 2019, Hikma Pharmaceuticals USA Inc.
Dunn KE, Finan PH, Tompkins DA, et al.: Characterizing pain and associated coping strategies in methadone and buprenorphine-maintained patients. Drug Alcohol Depend. 2015; 157: 143-149. DOI: 10.1016/j.drugalcdep.2015.10.018.
Gilam G, Sturgeon JA, You DS, et al.: Negative affect-related factors have the strongest association with prescription opioid misuse in a cross-sectional cohort of patients with chronic pain. Pain Med. 2020; 21(2): e127-e138. DOI: 10.1093/pm/pnz249.
Rosoff DB, Smith GD, Lohoff FW: Prescription opioid use and risk for major depressive disorder and anxiety and stress-related disorders: A multivariable mendelian randomization analysis. JAMA Psychiatry. 2021; 78(2): 151-160. DOI: 10.1001/jamapsychiatry.2020.3554.
Edwards AC, Larsson Lonn S, Sundquist J, et al.: Associations between divorce and onset of drug abuse in a Swedish national sample. Am J Epidemiol. 2018; 187(5): 1010-1018. DOI: 10.1093/aje/kwx321.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.