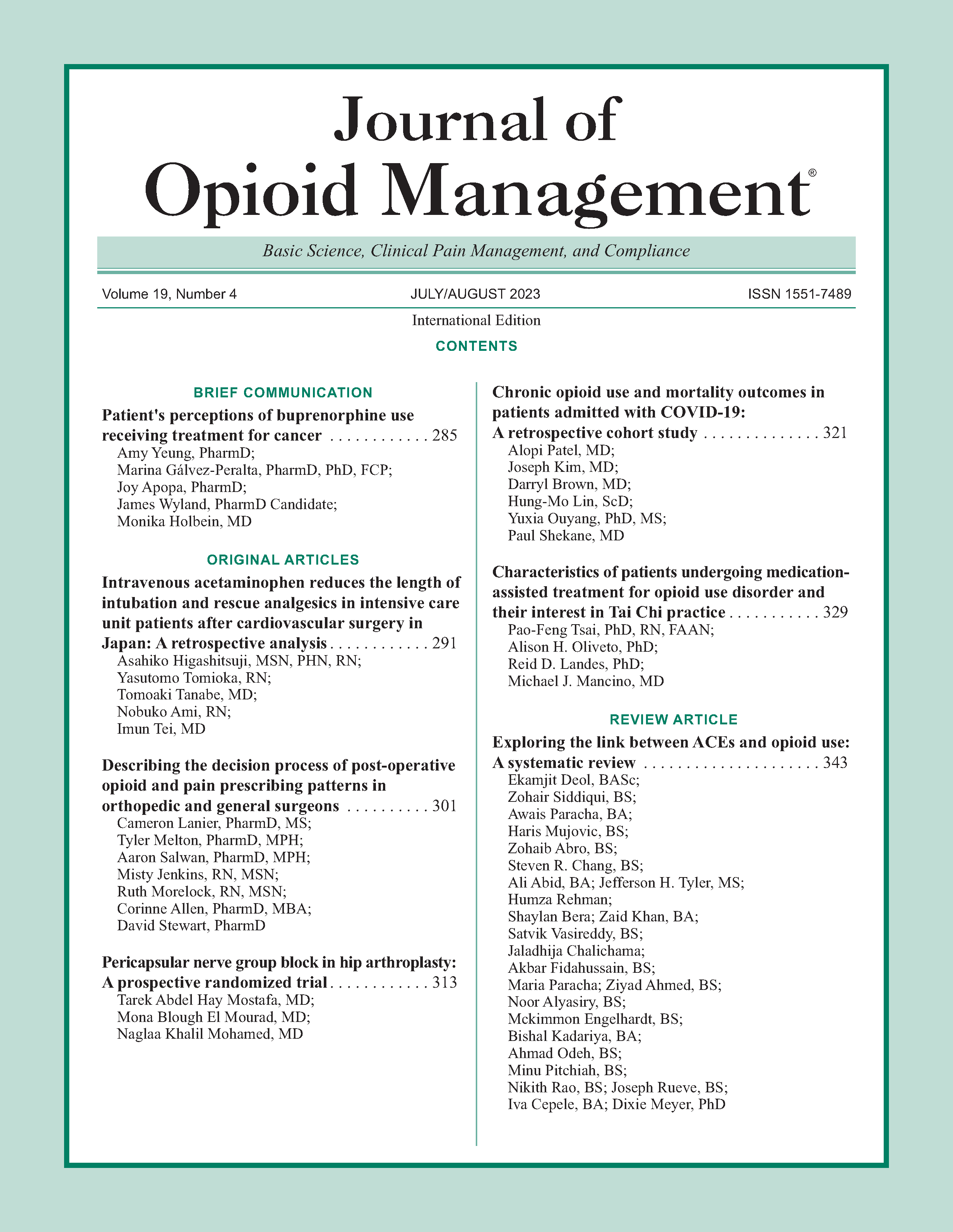
Exploring the link between ACEs and opioid use: A systematic review
DOI:
https://doi.org/10.5055/jom.2023.0791Keywords:
adverse childhood experience, opioid use disorder, opioid, opiate, child abuse, childhood traumaAbstract
Objective: To review the current literature surrounding the relationship between adverse childhood experiences (ACEs) and opioid use disorder (OUD) to guide clinical identification of high-risk individuals and assess treatment implications.
Design: A PubMed search was conducted from the year 2000 to 2022 using a series of primary and secondary search terms. A total of 21,524 unique results were screened for relevancy to ACEs and OUDs. After excluding unrelated articles, a total of 48 articles were included in this systematic review.
Results: Increased frequency of ACEs was directly related to increased risk of OUD and lower onset age. ACEs were also associated with OUD severity. ACEs linked to OUD included childhood neglect, emotional abuse, physical abuse, and sexual abuse. Additionally, dysfunctional childhood home environment, female gender, and psychiatric/behavioral comorbidities increased the risk of OUD, while resilience was found to be a protective factor. Multiple biochemical markers were associated with both ACEs and OUD.
Conclusions: Children experiencing multiple ACEs should be the target of preventative intervention by medical professionals. Clinicians should include ACEs in their opioid misuse risk assessment. High incidence of co-occurring psychiatric/behavioral disorders provides multiple treatment avenues for patients with OUD. Resilience, along with being therapy target, should be fostered early in the life course. Incorporation of family members may improve opioid abuse treatment outcomes. Future research should focus on interventions interrupting the progression of ACEs to OUD along with proposed biochemical pathways.
References
Dayer LE, Painter JT, McCain K, et al.: A recent history of opioid use in the US: Three decades of change. Subst Use Misuse. 2019; 54(2): 331-339.
Haley DF, Saitz R: The opioid epidemic during the COVID-19 pandemic. JAMA. 2020; 324(16): 1615-1617.
Manjiani D, Paul DB, Kunnumpurath S, et al.: Availability and utilization of opioids for pain management: Global issues. Ochsner J. 2014; 14(2): 208-215.
Lawrence Scholl PS, Kariisa M, Wilson N, et al.: Drug and opioid-involved overdose deaths—United States, 2013–2017. MMWR Morb Mort Wkly Rep. 2019; 67(5152): 1419-1427.
Slavova S, Rock P, Bush HM, et al.: Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020; 214: 108176-108176.
Douglas KR, Chan G, Gelernter J, et al.: Adverse childhood events as risk factors for substance dependence: Partial mediation by mood and anxiety disorders. Addict Behav. 2010; 35(1): 7-13.
Khoury L, Tang YL, Bradley B, et al.: Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depress Anxiety. 2010; 27(12): 1077-1086.
Groenewald CB, Murray CB, Palermo TM: Adverse childhood experiences and chronic pain among children and adolescents in the United States. Pain Rep. 2020; 5(5): e839-e839.
Darke S: Pathways to heroin dependence: Time to re-appraise self-medication. Addiction. 2013; 108(4): 659-667.
Rariden C, SmithBattle L, Yoo JH, et al.: Screening for adverse childhood experiences: Literature review and practice implications. J Nurse Pract. 2021; 17(1): 98-104.
Moher D, Liberati A, Tetzlaff J, et al.: The PG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLOS Med. 2009; 6(7): e1000097.
McManama O'Brien KH, Salas-Wright CP, Vaughn MG, et al.: Childhood exposure to a parental suicide attempt and risk for substance use disorders. Addict Behav. 2015; 46: 70-76.
Merrick MT, Ford DC, Haegerich TM, et al.: Adverse childhood experiences increase risk for prescription opioid misuse. J Prim Prev. 2020; 41(2): 139-152.
Forster M, Gower AL, Borowsky IW, et al.: Associations between adverse childhood experiences, student-teacher relationships, and non-medical use of prescription medications among adolescents. Addict Behav. 2017; 68: 30-34.
Barahmand U, Khazaee A, Hashjin GS: Emotion dysregulation mediates between childhood emotional abuse and motives for substance use. Arch Psychiatr Nurs. 2016; 30(6): 653-659.
Glavak R, Kuterovac-Jagodic G, Sakoman S: Perceived parental acceptance-rejection, family-related factors, and socioeconomic status of families of adolescent heroin addicts. Croat Med J. 2003; 44(2): 199-206.
Chiang S-C, Chen S-J, Sun H-J, et al.: Heroin use among youths incarcerated for illicit drug use: Psychosocial environment, substance use history, psychiatric comorbidity, and route of administration. Am J Addict. 2006; 15(3): 233-241.
Quinn K, Frueh BC, Scheidell J, et al.: Internalizing and externalizing factors on the pathway from adverse experiences in childhood to non-medical prescription opioid use in adulthood. Drug Alcohol Depend. 2019; 197: 212-219.
Wong CF, Silva K, Kecojevic A, et al.: Coping and emotion regulation profiles as predictors of nonmedical prescription drug and illicit drug use among high-risk young adults. Drug Alcohol Depend. 2013; 132(1-2): 165-171.
Swedo EA, Sumner SA, de Fijter S, et al.: Adolescent opioid misuse attributable to adverse childhood experiences. J Pediatr. 2020; 224: 102-109.e3.
Lei Y, Xi C, Li P, et al.: Association between childhood maltreatment and non-medical prescription opioid use among Chinese senior high school students: The moderating role of gender. J Affect Disord. 2018; 235: 421-427.
Mirhashem R, Allen HC, Adams ZW, et al.: The intervening role of urgency on the association between childhood maltreatment, PTSD, and substance-related problems. Addict Behav. 2017; 69: 98-103.
Engstrom M, El-Bassel N, Gilbert L: Childhood sexual abuse characteristics, intimate partner violence exposure, and psychological distress among women in methadone treatment. J Subst Abuse Treat. 2012; 43(3): 366-376.
Enoch M-A, Hodgkinson CA, Yuan Q, et al.: The influence of GABRA2, childhood trauma, and their interaction on alcohol, heroin, and cocaine dependence. Biol Psychiatry. 2010; 67(1): 20-27.
Lawson KM, Back SE, Hartwell KJ, et al.: A comparison of trauma profiles among individuals with prescription opioid, nicotine, or cocaine dependence. Am J Addict. 2013; 22(2): 127-131.
Cornford CS, Umeh K, Manshani N: Heroin users' experiences of depression: A qualitative study. Fam Pract. 2012; 29(5): 586-592.
Lovallo WR, Acheson A, Vincent AS, et al.: Early life adversity diminishes the cortisol response to opioid blockade in women: Studies from the family health patterns project. PLoS One. 2018; 13(10): e0205723-e0205723.
Afifi TO, Henriksen CA, Asmundson GJ, et al.: Childhood maltreatment and substance use disorders among men and women in a nationally representative sample. Can J Psychiatry. 2012; 57(11): 677-686.
Conroy E, Degenhardt L, Mattick RP, et al.: Child maltreatment as a risk factor for opioid dependence: Comparison of family characteristics and type and severity of child maltreatment with a matched control group. Child Abuse Negl. 2009; 33(6): 343-352.
Garland EL, Reese SE, Bedford CE, et al.: Adverse childhood experiences predict autonomic indices of emotion dysregulation and negative emotional cue-elicited craving among female opioid-treated chronic pain patients. Dev Psychopathol. 2019; 31(3): 1101-1110.
Derefinko KJ, Salgado García FI, Talley KM, et al.: Adverse childhood experiences predict opioid relapse during treatment among rural adults. Addict Behav. 2019; 96: 171-174.
Williams JR, Cole V, Girdler S, et al.: Exploring stress, cognitive, and affective mechanisms of the relationship between interpersonal trauma and opioid misuse. PLoS One. 2020; 15(5): e0233185.
Williams JR, Girdler S, Williams W, et al.: The effects of co-occurring interpersonal trauma and gender on opioid use and misuse. J Interpers Violence. 2021; 36(23-24): Np13185-Np13205.
Moselhy HF, Fahmy E, Mikhael VS, et al.: Impact of self-reported life events on the profile of opioid dependence syndrome. Am J Drug Alcohol Abuse. 2010; 36(1): 7-12.
Dawson-Rose C, Shehadeh D, Hao J, et al.: Trauma, substance use, and mental health symptoms in transitional age youth experiencing homelessness. Public Health Nurs. 2020; 37(3): 363-370.
Garami J, Valikhani A, Parkes D, et al.: Examining perceived stress, childhood trauma and interpersonal trauma in individuals with drug addiction. Psychol Rep. 2019; 122(2): 433-450.
Taplin C, Saddichha S, Li K, et al.: Family history of alcohol and drug abuse, childhood trauma, and age of first drug injection. Subst Use Misuse. 2014; 49(10): 1311-1316.
Moran L, Keenan E, Elmusharaf K: Barriers to progressing through a methadone maintenance treatment programme: Perspectives of the clients in the Mid-West of Ireland's drug and alcohol services. BMC Health Serv Res. 2018; 18(1): 911.
McDonnell E, Hevey D, McCauley M, et al.: Exploration of associations between early maladaptive schemas, impaired emotional regulation, coping strategies and resilience in opioid dependent poly-drug users. Subst Use Misuse. 2018; 53(14): 2320-2329.
McKernan LC, Nash MR, Gottdiener WH, et al.: Further evidence of self-medication: Personality factors influencing drug choice in substance use disorders. Psychodyn Psychiatry. 2015; 43(2): 243-275.
Roy A: Risk factors for attempting suicide in heroin addicts. Suicide Life Threat Behav. 2010; 40(4): 416-420.
Dangerfield DT, Heidari O, Cooper J, et al.: Motivations for opioid and stimulant use among drug using Black sexual minority men: A life course perspective. Drug Alcohol Depend.
; 215: 108224.
Carlyle M, Broomby R, Simpson G, et al.: A randomised, double-blind study investigating the relationship between early childhood trauma and the rewarding effects of morphine. Addict Biol. 2021; 26(6): e13047.
Guarino H, Mateu-Gelabert P, Quinn K, et al.: Adverse childhood experiences predict early initiation of opioid use behaviors. Front Sociol. 2021; 6: 620395.
Gannon M, Short V, LaNoue M, et al.: Prevalence of adverse childhood experiences of parenting women in drug treatment for opioid use disorder. Community Ment Health J. 2021; 57(5): 872-879.
Ag˘açhanlı R, Alnıak I · , Evren C: Sexual dysfunctions are predicted by childhood sexual abuse in women with opioid use disorder. Subst Use Misuse. 2018; 53(13): 2184-2189.
Peles E, Adelson M, Seligman Z, et al.: Psychiatric comorbidity differences between women with history of childhood sexual abuse who are methadone-maintained former opiate addicts and non-addicts. Psychiatry Res. 2014; 219(1): 191-197.
Schiff M, Levit S, Cohen-Moreno R: Childhood sexual abuse, post-traumatic stress disorder, and use of heroin among female clients in Israeli methadone maintenance treatment programs (MMTPS). Soc Work Health Care. 2010; 49(9): 799-813.
Li T, Du J, Yu S, et al.: Pathways to age of onset of heroin use: A structural model approach exploring the relationship of the COMT gene, impulsivity and childhood trauma. PLoS One. 2012; 7(11): e48735.
Wang Z, Du J, Sun H, et al.: Patterns of childhood trauma and psychological distress among injecting heroin users in China. PLoS One. 2010; 5(12): e15882-e15882.
Gerra G, Somaini L, Manfredini M, et al.: Dysregulated responses to emotions among abstinent heroin users: Correlation with childhood neglect and addiction severity. Prog Neuropsychopharmacol Biol Psychiatry. 2014; 48: 220-228.
Gerra LM, Gerra G, Mercolini L, et al.: Increased oxytocin levels among abstinent heroin addicts: Association with aggressiveness, psychiatric symptoms and perceived childhood neglect. Prog Neuropsychopharmacol Biol Psychiatry. 2017; 75: 70-76.
Khosravani V, Messman-Moore TL, Mohammadzadeh A, et al.: Effects of childhood emotional maltreatment on depressive symptoms through emotion dysregulation in treatment-seeking patients with heroin-dependence. J Affect Disord. 2019; 256: 448-457.
Rovisˇ D, Vasiljev V, Jenko-Prazˇnikar Z, et al.: Mental health and drug use severity: The role of substance P, neuropeptide Y, self-reported childhood history of trauma, parental bonding and current resiliency. J Ment Health. 2021; 30(1): 88-96.
Naqavi MR, Mohammadi M, Salari V, et al.: The relationship between childhood maltreatment and opiate dependency in adolescence and middle age. Addict Health. 2011; 3(3-4): 92-98.
Sun A-P, Chen Y-C, Marsiglia F: Trauma and Chinese heroin users. J Ethn Subst Abuse. 2016; 15(2): 144-159.
Ghorbani F, Khosravani V, Mohammadzadeh A, et al.: The role of emotion dysregulation in the relation of childhood trauma to heroin craving in individuals with heroin dependence. Drug Alcohol Depend. 2019; 195: 132-139.
Gerra G, Leonardi C, Cortese E, et al.: Adrenocorticotropic hormone and cortisol plasma levels directly correlate with childhood neglect and depression measures in addicted patients. Addict Biol. 2008; 13(1): 95-104.
Somer E, Altus L, Ginzburg K: Dissociative psychopathology among opioid use disorder patients: Exploring the “chemical dissociation” hypothesis. Compr Psychiatry. 2010; 51(4): 419-425.
Van den Berk-Clark C, Gallamore R, Barnes J, et al.: Identifying and overcoming barriers to trauma screening in the primary care setting. Families Syst Health. 2021; 39: 177-187.
Hancock C, Mennenga H, King N, et al.: Treating the rural opioid epidemic. National Rural Health Association Policy Brief. 2017; 1-13.
Christian CW: Committee on child A, neglect AAoP. The evaluation of suspected child physical abuse. Pediatrics. 2015; 135(5): e1337-1354.
Kumar N, Oles W, Howell BA, et al.: The role of social network support in treatment outcomes for medication for opioid use disorder: A systematic review. J Subst Abuse Treat. 2021; 127: 108367.
Sanders J, Munford R, Thimasarn-Anwar T, et al.: The role of positive youth development practices in building resilience and enhancing wellbeing for at-risk youth. Child Abuse Negl. 2015; 42: 40-53.
Rissanen I, Laine S, Puusepp I, et al.: Implementing and evaluating growth mindset pedagogy—A study of Finnish elementary school teachers. Front Educ. 2021; 6. DOI: 10.3389/feduc.2021.753698.
Campbell TL: Screening for adverse childhood experiences (ACEs) in primary care: A cautionary note. JAMA. 2020; 323(23): 2379-2380.
Chou R, Gordon DB, de Leon-Casasola OA, et al.: Management of postoperative pain: A clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine, and the American society of anesthesiologists. Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016; 17(2): 131-157.
Thiels CA, Anderson SS, Ubl DS, et al.: Wide variation and overprescription of opioids after elective surgery. Ann Surg. 2017; 266(4): 564-573.
Patwardhan A, Matika R, Gordon J, et al.: Exploring the role of chronic pain clinics: Potential for opioid reduction. Pain Phys. 2018; 21(6): E603-E610.
Battagliese G, Caccetta M, Luppino OI, et al.: Cognitive-behavioral therapy for externalizing disorders: A meta-analysis of treatment effectiveness. Behav Res Ther. 2015; 75: 60-71.
Cameron LD, Carroll P, Hamilton WK: Evaluation of an intervention promoting emotion regulation skills for adults with persisting distress due to adverse childhood experiences. Child Abuse Negl. 2018; 79: 423-433.
MacIsaac A, Mushquash AR, Mohammed S, et al.: Adverse childhood experiences and building resilience with the JoyPop app: Evaluation study. JMIR Mhealth Uhealth. 2021; 9(1): e25087.
Al Ghafri H, Hasan N, Elarabi HF, et al.: The impact of family engagement in opioid assisted treatment: Results from a randomized controlled trial. Int J Soc Psychiatry. 2022; 68(1): 166-170.
Amaechi O, Rodriguez JE: Minority physicians are not protected by their white coats. Fam Med. 2020; 52(8): 603.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.