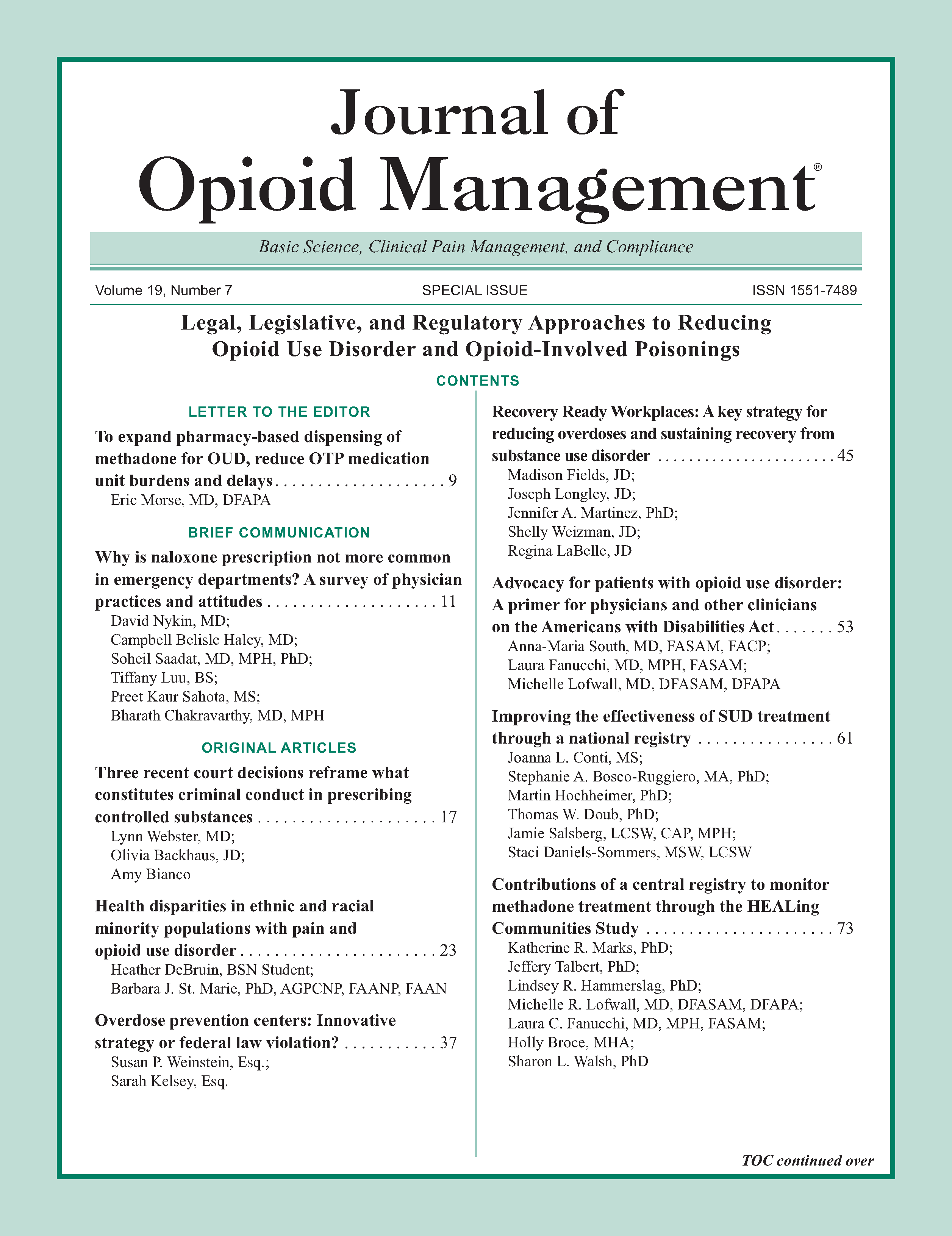
Contributions of a central registry to monitor methadone treatment through the HEALing Communities Study
DOI:
https://doi.org/10.5055/jom.2023.0801Keywords:
Helping to End Addiction Long-term, National Institutes of Health Helping to End Addiction Long-term Initiative, methadone, opioid use disorder, central registryAbstract
Objective: To describe the process of establishing a Methadone Central Registry (MCR) as part of the HEALing (Helping to End Addiction Long-termSM) Communities Study (HCS) and to support recommendations with evidence of its functionality relative to Medicaid claims data for monitoring utilization of methadone, an evidence-based treatment for opioid use disorder.
Design and participants: The manuscript authors were active participants in establishing the MCR and include representation from state government, Opioid Treatment Programs (OTPs), and HCS university partners. Secondary data were obtained from Kentucky's (KY's) MCR and Medicaid claims from July 2020 through June 2021. The functionality of data obtained from the MCR, as measured by data completeness and timeliness, is compared with Medicaid claims, the current standard.
Main outcomes: Central registry and Medicaid data were each aggregated statewide and at the HCS-KY county level. Dual levels of analysis were selected to inform stakeholders at the study and state levels. Descriptive statistics were calculated for the number of patients in methadone treatment.
Results: Statewide, the MCR provided a daily record of all individuals receiving methadone through an OTP within 72 hours. In contrast, Medicaid claims processing lagged 9 months and captured 57-62 percent of patients in the MCR.
Conclusions: Replacing a fax-based system, an MCR meets the converging need of providers, regulatory authorities, and researchers to monitor utilization, patient dual enrollment, and treatment outcomes. Implementation strategies included key stakeholder engagement, state partner leadership, training, and federal funding. Adoption of an MCR is recommended.
References
Ahmad FB, Rossen LM, Sutton P: Provisional drug overdose death counts. 2021. Available at https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed April 15, 2022.
Slavova S, Rock P, Bush HM, et al.: Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020; 214: 108176. DOI: 10.1016/j.drugalcdep.2020.108176. DOI: https://doi.org/10.1016/j.drugalcdep.2020.108176
Slavova S, Quesinberry D, Hargrove S, et al.: Trends in drug overdose mortality rates in Kentucky, 2019-2020. JAMA Netw Open. 2021; 4(7): e2116391. DOI: 10.1001/jamanetworkopen.2021.16391. DOI: https://doi.org/10.1001/jamanetworkopen.2021.16391
Larochelle MR, Bernson D, Land T, et al.: Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: A cohort study. Ann Intern Med. 2018; 169(3): 137-145. DOI: 10.7326/m17-3107. DOI: https://doi.org/10.7326/M17-3107
HEALing Communities Study Consortium: The HEALing (helping to end addiction long-termSM) Communities Study: Protocol for a cluster randomized trial at the community level to reduce opioid overdose deaths through implementation of an integrated set of evidence-based practices. Drug Alcohol Depend. 2020; 217: 108335. DOI: 10.1016/j.drugalcdep.2020.108335. DOI: https://doi.org/10.1016/j.drugalcdep.2020.108335
Knudsen HK, Drainoni ML, Gilbert L, et al.: Model and approach for assessing implementation context and fidelity in the HEALing Communities Study. Drug Alcohol Depend. 2020; 217: 108330. DOI: 10.1016/j.drugalcdep.2020.108330. DOI: https://doi.org/10.1016/j.drugalcdep.2020.108330
Glasgow RE, Harden SM, Gaglio B, et al.: RE-AIM planning and evaluation framework: Adapting to new science and practice with a 20-year review. Front Public Health. 2019; 7: 64. DOI: 10.3389/fpubh.2019.00064. DOI: https://doi.org/10.3389/fpubh.2019.00064
Winhusen T, Walley A, Fanucchi LC, et al.: The opioid-overdose reduction continuum of care approach (ORCCA): Evidence-based practices in the HEALing Communities Study. Drug Alcohol Depend. 2020; 217: 108325. DOI: 10.1016/j.drugalcdep.2020.108325. DOI: https://doi.org/10.1016/j.drugalcdep.2020.108325
Substance Abuse and Mental Health Services Administration: NSDUH Series H-54. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality (Substance Abuse and Mental Health Services Administration), 2019.
Wu LT, Zhu H, Swartz MS: Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2016; 169: 117-127. DOI: 10.1016/j.drugalcdep.2016.10.015. DOI: https://doi.org/10.1016/j.drugalcdep.2016.10.015
Sordo L, Barrio G, Bravo MJ, et al.: Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. BMJ. 2017; 357: J1550. DOI: 10.1136/bmj.j1550. DOI: https://doi.org/10.1136/bmj.j1550
Morgan JR, Schackman BR, Weinstein ZM, et al.: Overdose following initiation of naltrexone and buprenorphine medication treatment for opioid use disorder in a United States commercially insured cohort. Drug Alcohol Depend. 2019; 200: 34-39. DOI: 10.1016/j.drugalcdep.2019.02.031. DOI: https://doi.org/10.1016/j.drugalcdep.2019.02.031
Jarvis BP, Holtyn AF, Subramaniam S, et al.: Extended-release injectable naltrexone for opioid use disorder: A systematic review. Addiction. 2018; 113(7): 1188-1209. DOI: 10.1111/add.14180. DOI: https://doi.org/10.1111/add.14180
Wakeman SE, Larochelle MR, Ameli O, et al.: Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open. 2020; 3(2): e1920622-e1920622. DOI: 10.1001/jamanetworkopen.2019.20622. DOI: https://doi.org/10.1001/jamanetworkopen.2019.20622
US Health and Human Services Department: Confidentiality of Substance Use Disorder Patient Records. Washington, DC: Substance Abuse and Mental Health Services Administration, US Health and Human Services Department, 2017.
US Health and Human Services Department: Confidentiality of Substance Use Disorder Patient Records. Washington, DC: Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services, 2020.
Nosyk B, Anglin MD, Brissette S, et al.: A call for evidence-based medical treatment of opioid dependence in the United States and Canada. Health Aff (Millwood). 2013; 32(8): 1462-1469. DOI: 10.1377/hlthaff.2012.0846. DOI: https://doi.org/10.1377/hlthaff.2012.0846
Sprague Martinez L, Rapkin BD, Young A, et al.: Community engagement to implement evidence-based practices in the HEALing Communities Study. Drug Alcohol Depend. 2020; 217: 108326. DOI: 10.1016/j.drugalcdep.2020.108326. DOI: https://doi.org/10.1016/j.drugalcdep.2020.108326
Slavova S, LaRochelle MR, Root ED, et al.: Operationalizing and selecting outcome measures for the HEALing Communities Study. Drug Alcohol Depend. 2020; 217: 108328. DOI: 10.1016/j.drugalcdep.2020.108328. DOI: https://doi.org/10.1016/j.drugalcdep.2020.108328
US Census Bureau: Kentucky state profile. Available at https://www.census.gov/library/stories/state-by-state/kentucky-population-change-between-census-decade.html. Accessed January 25, 2023.
Kentucky Department of Medicaid Services: Department for Medicaid services monthly membership counts by county. 2021. Available at https://www.chfs.ky.gov/agencies/dms/stats/KYDWMMCC022022.pdf. Accessed December 29, 2022.
An act requiring certain reports for opiate overdoses: Chapter 55, 191st Leg (Mass 2015). 2015. Available at https://malegislature.gov/Laws/SessionLaws/Acts/2015/Chapter55. Accessed December 29, 2022.
Substance Abuse and Mental Health Services Administration, HHS. Fact Sheet: SAMHSA 42 CFR Part 2 Revised Rule. 2020. Available at https://www.samhsa.gov/newsroom/pressannouncements/202007131330. Accessed December 29, 2022.
Lighthouse Software Systems: The Central Registry. Available at https://www.lhss.net/central-registry. Accessed December 29, 2022.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.