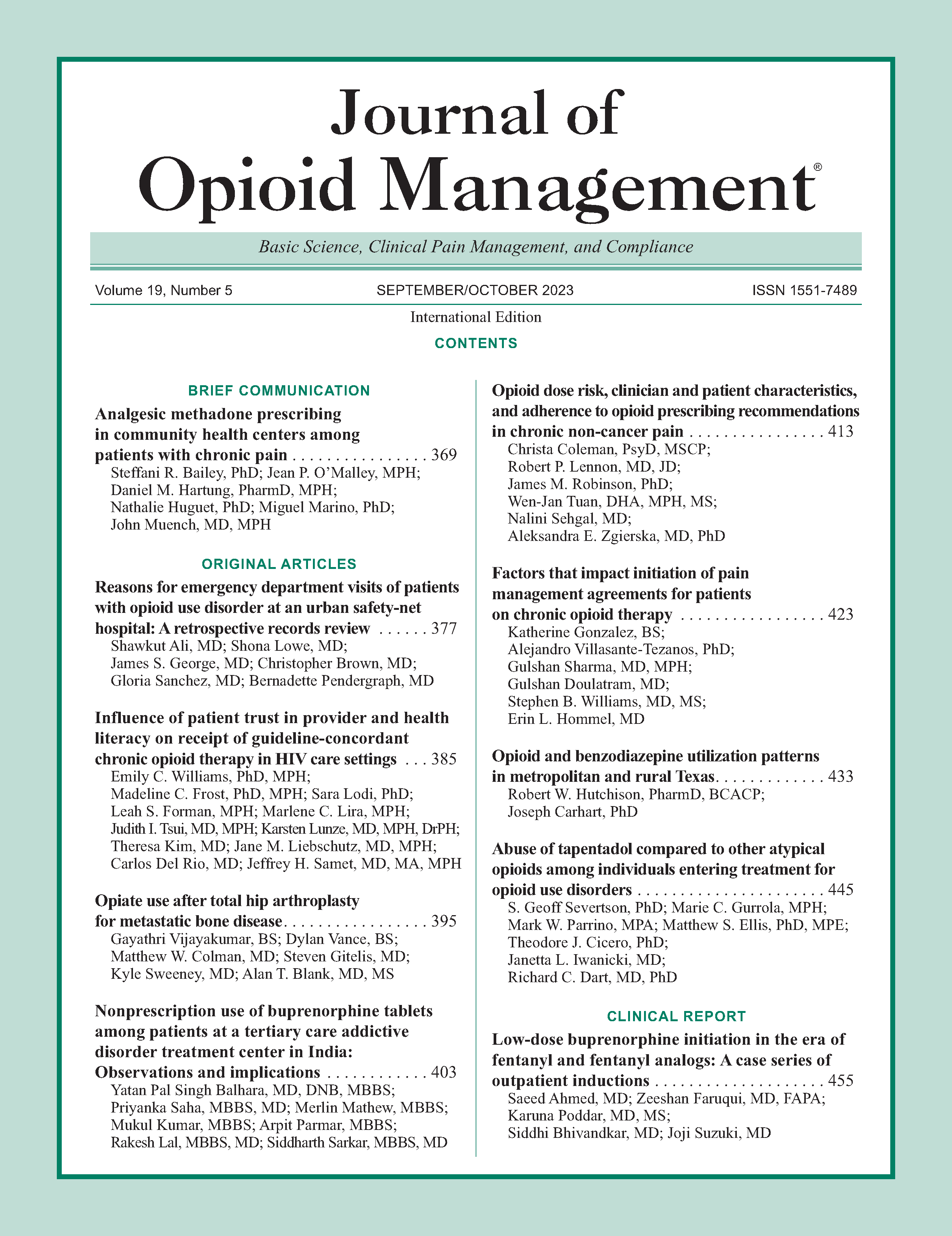
Factors that impact initiation of pain management agreements for patients on chronic opioid therapy
DOI:
https://doi.org/10.5055/jom.0816Keywords:
pain management agreement, chronic pain, opioid therapyAbstract
Objective: This analysis seeks to understand variables within our institution that impact pain management agreement (PMA) utilization for chronic noncancer pain (CNCP).
Design: Retrospective chart review.
Setting: Public academic medical center.
Patients: Adults prescribed an opioid for CNCP between July 2020 and October 2020.
Main outcome measure: We assessed the association between patient demographics, prescription factors, and prescriber factors with the presence of a PMA. Unadjusted rates and chi-square tests were generated for each predictor. Additionally, we performed two multivariable logistic regressions: one including all variables and another utilizing a stepwise forward variable selection process to further understand the relationships between predictors and the presence of a PMA.
Results: 49.7 percent of patients who received an opioid for CNCP had a PMA on file. One significant predictor of the presence of PMA was prescriber specialty with anesthesia/pain medicine, demonstrating 88 percent compliance. Compared to anesthesia/pain medicine, patients receiving opioids from internal medicine had an odds ratio (OR) of 0.155 (95 percent confidence interval (CI), 0.109-0.220), while patients receiving opioids from family medicine had an OR of 0.122 (95 percent CI, 0.090-0.167). Additionally, patients who received schedule II opioids (as opposed to schedule III/IV opioids), patients with multiple opioid fills in 3 months, middle aged patients, and Black patients were more likely to have a PMA.
Conclusions: Compliance with PMA within our institution was only 49 percent despite an existing state law mandating use. Our analysis suggests quality improvement interventions should target patients on schedule III/IV opioids who receive their prescriptions from primary care providers.
References
Centers for Medicare and Medicaid Services: CMS roadmap strategy to fight the opioid crisis. Available at https://www.cms.gov/About-CMS/Agency-Information/Emergency/Downloads/Opioid-epidemic-roadmap.pdf. Accessed February 6, 2022.
Chou R, Fanciullo GJ, Fine PG, et al.: Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009; 10: 113-130.e22. DOI: https://doi.org/10.1016/j.jpain.2008.10.008
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016; 315: 1624-1645. DOI: https://doi.org/10.1001/jama.2016.1464
Federation of State Medical Boards: Guidelines for the chronic use of opioid analgesics. Available at https://www.fsmb.org/siteassets/advocacy/policies/opioid_guidelines_as_adopted_april-2017_final.pdf. Accessed February 6, 2022.
Teitelbaum J, Rosenbaum S: Gonzales v. Oregon: Implications for public health policy and practice. Public Health Rep. 2007; 122: 122-124. DOI: https://doi.org/10.1177/003335490712200117
Federation of State Medical Boards: Pain management policies board by board overview. Available at https://www.fsmb.org/siteassets/advocacy/key-issues/pain-management-by-state.pdf. Accessed February 6, 2022.
National Alliance for Model State Drug Laws: Overview of state pain management and prescribing policies. Available at https://namsdl.org/wp-content/uploads/Overview-of-State-Pain-Management-and-Prescribing-Policies-1.pdf. Accessed February 6, 2022.
Texas Administrative Code: Rule 1703 minimum requirements for the treatment of chronic pain. Available at https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=R&app=9&p_dir=&p_rloc=&p_tloc=&p_ploc=&pg=1&p_tac=&ti=22&pt=9&ch=170&rl=3. Accessed February 6, 2022.
Wong R, Carroll W, Muttreja A, et al.: Improving opioid management and resource utilization in an internal medicine residency clinic: A before-after study over two plan-do-study-act cycles. Pain Med. 2019; 20: 1919-1924. DOI: https://doi.org/10.1093/pm/pny239
Kay C, Wozniak E, Koller S, et al.: Adherence to chronic opioid therapy prescribing guidelines in a primary care clinic. J Opioid Manag. 2016; 12: 333-345. DOI: https://doi.org/10.5055/jom.2016.0350
Kay C, Wozniak E, Ching A, et al.: Pain agreements and healthcare utilization in a veterans affairs primary care population: A retrospective chart review. Pain Ther. 2018; 7: 121-126. DOI: https://doi.org/10.1007/s40122-018-0098-5
Texas Administrative Code: Prescription of controlled substances pain management definitions rule 1702. Available at https://texreg.sos.state.tx.us/public/readtac$ext.TacPage?sl=R&app=9&p_dir=&p_rloc=&p_tloc=&p_ploc=&pg=1&p_tac=&ti=22&pt=9&ch=170&rl=2. Accessed February 6, 2022.
United States Drug Enforcement Administration: Drug scheduling. Available at https://www.dea.gov/drug-information/drug-scheduling. Accessed February 6, 2022.
Oregon Pain Guidance: Opioid conversion calculator. Available at https://www.oregonpainguidance.org/opioidmedcalculator/. Accessed February 6, 2022.
Substance Abuse and Mental Health Services Administration: Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. Available at https://www.samhsa.gov/data/report/2017-nsduh-annual-national-report. Accessed February 6, 2022.
Breuer B, Cruciani R, Portenoy RK: Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: A national survey. South Med J. 2010; 103: 738-747. DOI: https://doi.org/10.1097/SMJ.0b013e3181e74ede
Fishman SM, Mahajan G, Jung SW, et al.: The trilateral opioid contract bridging the pain clinic and the primary care physician through the opioid contract. J Pain Symptom Manage. 2002; 24: 335-344. DOI: https://doi.org/10.1016/S0885-3924(02)00486-4
Laks J, Alford DP, Patel K, et al.: A national survey on patient provider agreements when prescribing opioids for chronic pain. J Gen Intern Med. 2021; 36: 600-605. DOI: https://doi.org/10.1007/s11606-020-06364-2
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.