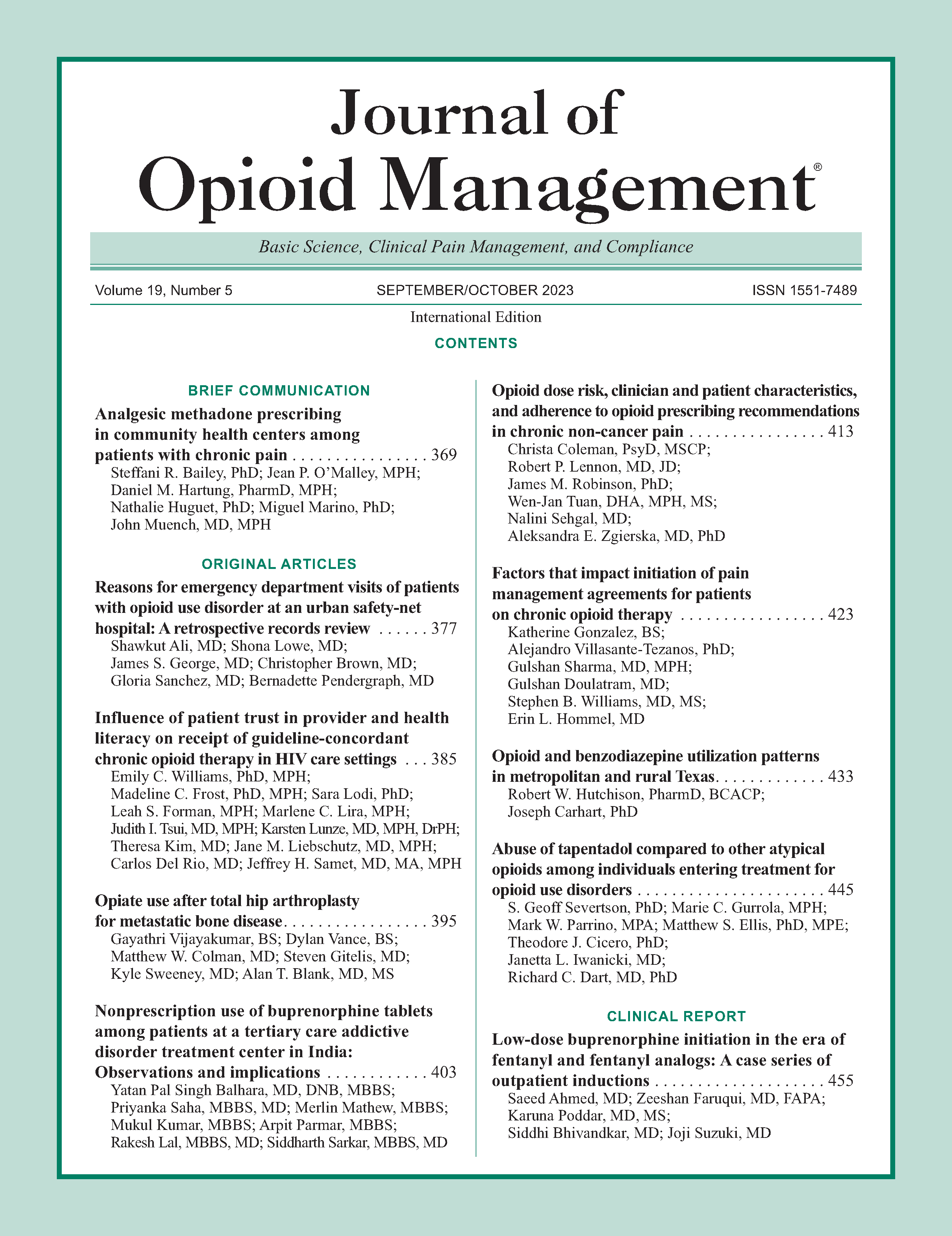
Opioid and benzodiazepine utilization patterns in metropolitan and rural Texas
DOI:
https://doi.org/10.5055/jom.0817Keywords:
opioid, benzodiazepine, metropolitan, rural, PDMPAbstract
Introduction: Although many drugs are implicated in the crisis, opioids and concomitant sedatives are associated with increased overdose risk in both rural and urban communities. Individuals in rural areas are up to 5-fold more likely to experience adverse outcomes related to opioids. The primary objective of this study was to evaluate concomitant use of opioid and benzodiazepine prescriptions in Texas, compare metropolitan and rural differences, and use these data to inform clinicians and to help develop harm reduction strategies.
Methods: Prescribing data were extracted from the Texas Prescription Drug Monitoring Program (PDMP) public use data file, the statewide monitoring program administered by the Texas State Board of Pharmacy. An overlapping drug combination prescription day was defined as any day in which a patient had at least one of the overlapping drug types—eg, opioid + benzodiazepine, opioid + benzodiazepine + carisoprodol.
Results: In Texas, 47.4 percent of the counties with the highest number of overlapping days (per patient) bordered other states. Providers who practice in rural areas prescribe opioid and benzodiazepine medications with 8.2 more overlapping days per quarter.
Discussion: Taking both opioid and benzodiazepine prescriptions is associated with increased overdose risk. Opioid prescription data provide a distinct view into the opioid epidemic that allows all states and counties to view the trends of opioid utilization. There are only a few studies using PDMP data to compare urban and rural trends.
Conclusions: Rural patients had more benzodiazepine and opioid days overlap than urban patients. The prevalence is higher among older adults and providers who practice in rural areas (average 8.2 more days per quarter). Our findings in Texas indicate a trend downward in overlap for both rural and urban areas over the last year of measurement. However, rural areas are still significantly higher.
References
Hedegaard H, Spencer MR: Drug overdose deaths in the United States, 1999-2020. NCHS Data Brief. 2021; 426: 1-8. DOI: https://doi.org/10.15620/cdc:112340
Havens JR, Oser CB, Leukefeld CG: Differences in prevalence of prescription opiate misuse among rural and urban probationers. Am J Drug Alcohol Abuse. 2007; 33(2): 309-317. DOI: https://doi.org/10.1080/00952990601175078
CDC: Drug Overdose Deaths in the US Top 100,000 Annually, in CDC Newsletter. 2021. Atlanta, GA: Center for Disease Control.
Hwang CS, Kang EM, Kornegay CJ, et al.: Trends in the concomitant prescribing of opioids and benzodiazepines, 2002-2014. Am J Prev Med. 2016; 51(2): 151-160. DOI: https://doi.org/10.1016/j.amepre.2016.02.014
Hedegaard H, Spencer MR: Urban-rural differences in drug overdose death rates, 1999-2019. NCHS Data Brief. 2021; 403: 1-8. DOI: https://doi.org/10.15620/cdc:102891
Altekruse SF, Cosgrove CM, Altekruse WC, et al.: Socioeconomic risk factors for fatal opioid overdoses in the United States: Findings from the mortality disparities in American Communities Study (MDAC). PLoS One. 2020; 15(1): e0227966. DOI: https://doi.org/10.1371/journal.pone.0227966
Cragg A, Hau JP, Woo SA, et al.: Risk factors for misuse of prescribed opioids: A systematic review and meta-analysis. Ann Emerg Med. 2019; 74(5): 634-646. DOI: https://doi.org/10.1016/j.annemergmed.2019.04.019
Centers for Disease Control and Prevention: Opioid Dispensing Rate Maps. Atlanta, GA: National Center for Injury Prevention and Control, 2021.
Hutchison RW, Carhart JW, Holloway K: Texas prescription drug monitoring program evolution and outcomes. Texas J Health-Syst Pharm. 2021; 20(2): 22-27.
Gabay M: The federal controlled substances act: Schedules and pharmacy registration. Hosp Pharm. 2013; 48(6): 473-474. DOI: https://doi.org/10.1310/hpj4806-473
DasGupta D: The Urban/Rural Divide in Access to Medication-Assisted Treatment for Opioid Use Disorder in Utah. Utah State University Extension, 2020.
Johnson Q, Mund B, Joudrey PJ: Improving rural access to opioid treatment programs. J Law Med Ethics. 2018; 46(2): 437-439. DOI: https://doi.org/10.1177/1073110518782951
Sears JM, Haight JR, Fulton-Kehoe D, et al.: Changes in early high-risk opioid prescribing practices after policy interventions in Washington state. Health Serv Res. 2021; 56(1): 49-60. DOI: https://doi.org/10.1111/1475-6773.13564
Luu H, Slavova S, Freeman PR, et al.: Trends and patterns of opioid analgesic prescribing: Regional and rural-urban variations in Kentucky from 2012 to 2015. J Rural Health. 2019; 35(1): 97-107. DOI: https://doi.org/10.1111/jrh.12300
Carlson A, Nelson ME, Patel H: Longitudinal impact of a pre-populated default quantity on emergency department opioid prescriptions. J Am Coll Emerg Physicians Open. 2021; 2(1): e12337. DOI: https://doi.org/10.1002/emp2.12337
Funmaker W: Opioid data surveillance report. Great Lakes Inter-Tribal Epidemiology Center (GLITEC). 2020. 17. Kim HS, McCarthy DM, Courtney DM, et al.: Benzodiazepine-opioid co-prescribing in a national probability sample of ED encounters. Am J Emerg Med. 2017; 35(3): 458-464. DOI: https://doi.org/10.1016/j.ajem.2016.11.054
McClure FL, Niles JK, Kaufman HW, et al.: Concurrent use of opioids and benzodiazepines: Evaluation of prescription drug monitoring by a United States laboratory. J Addict Med. 2017; 11(6): 420-426. DOI: https://doi.org/10.1097/ADM.0000000000000354
Shah A, Hayes CJ, Martin BC: Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017; 66(10): 265-269. DOI: https://doi.org/10.15585/mmwr.mm6610a1
Sun EC, Dixit A, Humphreys K, et al.: Association between concurrent use of prescription opioids and benzodiazepines and overdose: Retrospective analysis. BMJ. 2017; 356: J760. DOI: https://doi.org/10.1136/bmj.j760
Cho J, Spence MM, Niu F, et al.: Risk of overdose with exposure to prescription opioids, benzodiazepines, and non-benzodiazepine sedative-hypnotics in adults: A retrospective cohort study. J Gen Intern Med. 2020; 35(3): 696-703. DOI: https://doi.org/10.1007/s11606-019-05545-y
Adams RS, Corrigan JD, Ritter GA, et al.: Association of lifetime history of traumatic brain injury with prescription opioid use and misuse among adults. J Head Trauma Rehabil. 2021; 36(5): 328-337. DOI: https://doi.org/10.1097/HTR.0000000000000729
Lund BC, Ohl ME, Hadlandsmyth K, et al.: Regional and rural–urban variation in opioid prescribing in the veterans health administration. Mil Med. 2019; 184(11-12): 894-900. DOI: https://doi.org/10.1093/milmed/usz104
Sande K: Barriers to MOUD in rural areas. RHIhub. 2021. Available at www.ruralhealthinfo.org/toolkits/moud/1/barriers. Accessed July 20, 2023.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.