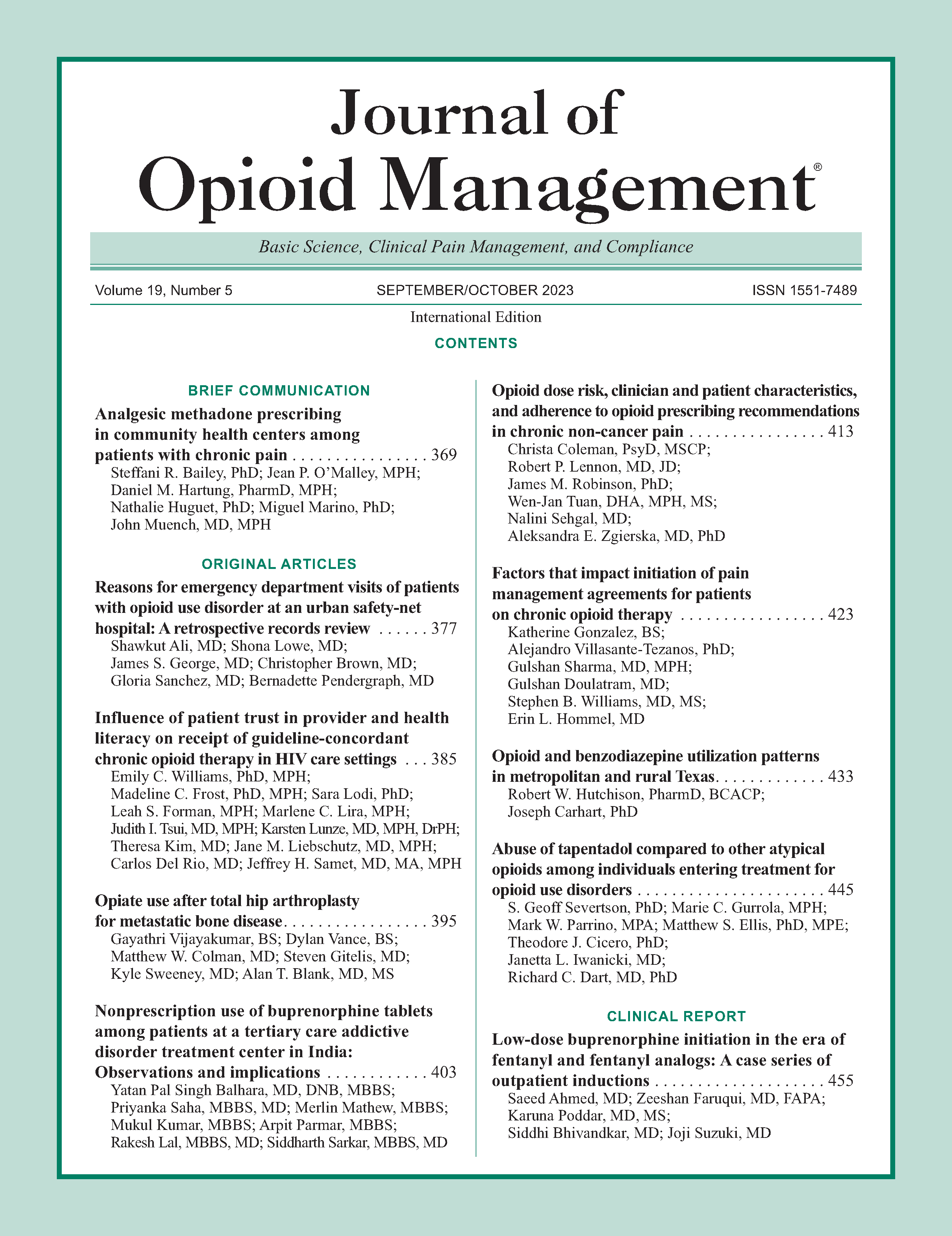
Low-dose buprenorphine initiation in the era of fentanyl and fentanyl analogs: A case series of outpatient inductions
DOI:
https://doi.org/10.5055/jom.0819Keywords:
buprenorphine, naloxone, microinduction, microdosing, buprenorphine/naloxone, low-dose buprenorphineAbstract
Buprenorphine, a partial opioid agonist, is a Food and Drug Administration-approved medication for the treatment of opioid use disorder (OUD). However, due to its high binding affinity, precipitated withdrawal may occur if initiated in the presence of other opioids. The growing literature demonstrates promise for alternative induction model of low-dose initiation of buprenorphine for the treatment of OUD, specifically targeting patients averse to withdrawal or using fentanyl. In this case series, we present four clinical cases of outpatient inductions, in which three out of four successfully transitioned from fentanyl to buprenorphine, and one patient transitioned from methadone to buprenorphine using a low-dose induction method.
References
National Center for Health Statistics: Drug overdose deaths in the US top 100 annually, GA: US Department of Health and Human Services, CDC. 2021. Available at https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20210714.htm. Accessed July 2021.
Florence C, Luo F, Rice K: The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug Alcohol Depend. 2021; 218: 108350. DOI: https://doi.org/10.1016/j.drugalcdep.2020.108350
US Food and Drug Administration: Information about medication-assisted treatment (MAT). 2019; 14: 758-768. Available at https://www.fda.gov/drugs/information-drugclass/information-about-medication-assisted-treatment-mat. Accessed June 30, 2023.
Sordo L, Barrio G, Bravo MJ, et al.: Mortality risk during and after opioid substitution treatment: Systematic review and meta-analysis of cohort studies. BMJ. 2017; 357: j1550. DOI: 10.1136/bmj.j1550. DOI: https://doi.org/10.1136/bmj.j1550
Wakeman SE, Larochelle MR, Ameli O, et al.: Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open. 2020; 3(2): e1920622-e1920622. DOI: https://doi.org/10.1001/jamanetworkopen.2019.20622
Lister JJ, Weaver A, Ellis JD, et al.: A systematic review of rural-specific barriers to medication treatment for opioid use disorder in the United States. Am J Drug Alcohol Abuse. 2020; 46(3): 273-288. DOI: https://doi.org/10.1080/00952990.2019.1694536
Cioe K, Biondi BE, Easly R, et al.: A systematic review of patients' and providers' perspectives of medications for treatment of opioid use disorder. J Subst Abuse Treat. 2020; 119: 108146. DOI: https://doi.org/10.1016/j.jsat.2020.108146
Medicine ASoA: The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med. 2020; 14(2S): 1-91. DOI: https://doi.org/10.1097/ADM.0000000000000633
McCance-Katz E, Johnson K, Harding F, et al.: Medications for opioid use disorder-TIP 63. SAMSHA. 2018; 3-62.
Hämmig R, Kemter A, Strasser J, et al.: Use of microdoses for induction of buprenorphine treatment with overlapping full opioid agonist use: The Bernese method. Subst Abuse Rehabil. 2016; 7: 99. DOI: https://doi.org/10.2147/SAR.S109919
Ahmed S, Bhivandkar S, Lonergan BB, et al.: Microinduction of buprenorphine/naloxone: A review of the literature. Am J Addict. 2021; 30(4): 305-315. DOI: https://doi.org/10.1111/ajad.13135
Wong JS, Nikoo M, Westenberg JN, et al.: Comparing rapid micro-induction and standard induction of buprenorphine/naloxone for treatment of opioid use disorder: Protocol for an openlabel, parallel-group, superiority, randomized controlled trial. Addict Sci Clin Pract. 2021; 16(1): 1-10. DOI: https://doi.org/10.1186/s13722-021-00220-2
Varshneya NB, Thakrar AP, Hobelmann JG, et al.: Evidence of buprenorphine-precipitated withdrawal in persons who use fentanyl. J Addict Med. 2022; 16(4): e265-e268. DOI: https://doi.org/10.1097/ADM.0000000000000922
Randhawa PA, Brar R, Nolan S: Buprenorphine–naloxone “microdosing”: An alternative induction approach for the treatment of opioid use disorder in the wake of North America's increasingly potent illicit drug market. CMAJ. 2020; 192(3): E73-E73. DOI: https://doi.org/10.1503/cmaj.74018
Weimer MB, Fiellin DA: Low- and very low-dose buprenorphine induction: New (ish) uses for an old (ish) medication? Addiction. 2022; 117(6): 1507-1509. DOI: https://doi.org/10.1111/add.15799
Hämmig R: Einleitung einer substitutionsbehandlung mit buprenorphin unter vorübergehender überlappung mit heroinkonsum: Ein neuer ansatz (“berner methode”). Suchttherapie. 2010; 11(3): 129-132. DOI: https://doi.org/10.1055/s-0030-1261914
Terasaki D, Smith C, Calcaterra SL: Transitioning hospitalized patients with opioid use disorder from methadone to buprenorphine without a period of opioid abstinence using a microdosing protocol. Pharmacotherapy. 2019; 39(10): 1023-1029. DOI: https://doi.org/10.1002/phar.2313
Robbins JL, Englander H, Gregg J: Buprenorphine microdose induction for the management of prescription opioid dependence. J Am Board Fam. 2021; 34(Suppl): S141-S146. DOI: https://doi.org/10.3122/jabfm.2021.S1.200236
Thakrar AP, Jablonski L, Ratner J, et al.: Micro-dosing intravenous buprenorphine to rapidly transition from full opioid agonists. J Addict Med. 2022; 16(1): 122-124. DOI: https://doi.org/10.1097/ADM.0000000000000838
Klaire S, Zivanovic R, Barbic SP, et al.: Rapid micro-induction of buprenorphine/naloxone for opioid use disorder in an inpatient setting: A case series. Am J Addict. 2019; 28(4): 262-265. DOI: https://doi.org/10.1111/ajad.12869
Brar R, Fairbairn N, Sutherland C, et al.: Use of a novel prescribing approach for the treatment of opioid use disorder: Buprenorphine/naloxone micro-dosing—A case series. Drug Alcohol Rev. 2020; 39(5): 588-594. DOI: https://doi.org/10.1111/dar.13113
Suen LW, Lee TG, Silva M, et al.: Rapid overlap initiation protocol using low dose buprenorphine for opioid use disorder treatment in an outpatient setting: A case series. J Addict Med. 2022; 16: 534-540. DOI: https://doi.org/10.1097/ADM.0000000000000961
Weiss RD, Potter JS, Fiellin DA, et al.: Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: A 2-phase randomized controlled trial. Arch Gen Psychiatry. 2011; 68(12): 1238-1246. DOI: https://doi.org/10.1001/archgenpsychiatry.2011.121
Dugosh K, Abraham A, Seymour B, et al.: A systematic review on the use of psychosocial interventions in conjunction with medications for the treatment of opioid addiction. J Addict Med. 2016; 10(2): 91. DOI: https://doi.org/10.1097/ADM.0000000000000193
National Institute on Drug Abuse: Principles of drug addiction treatment: A research-based guide. National Institute on Drug Abuse, National Institutes of Health, 2018.
McHugh RK, Hearon BA, Otto MW: Cognitive behavioral therapy for substance use disorders. Psychiatric Clinics. 2010; 33(3): 511-525. DOI: https://doi.org/10.1016/j.psc.2010.04.012
Miller WR, Rollnick S: Motivational interviewing: Helping people change. New York: Guilford Press, 2012.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.