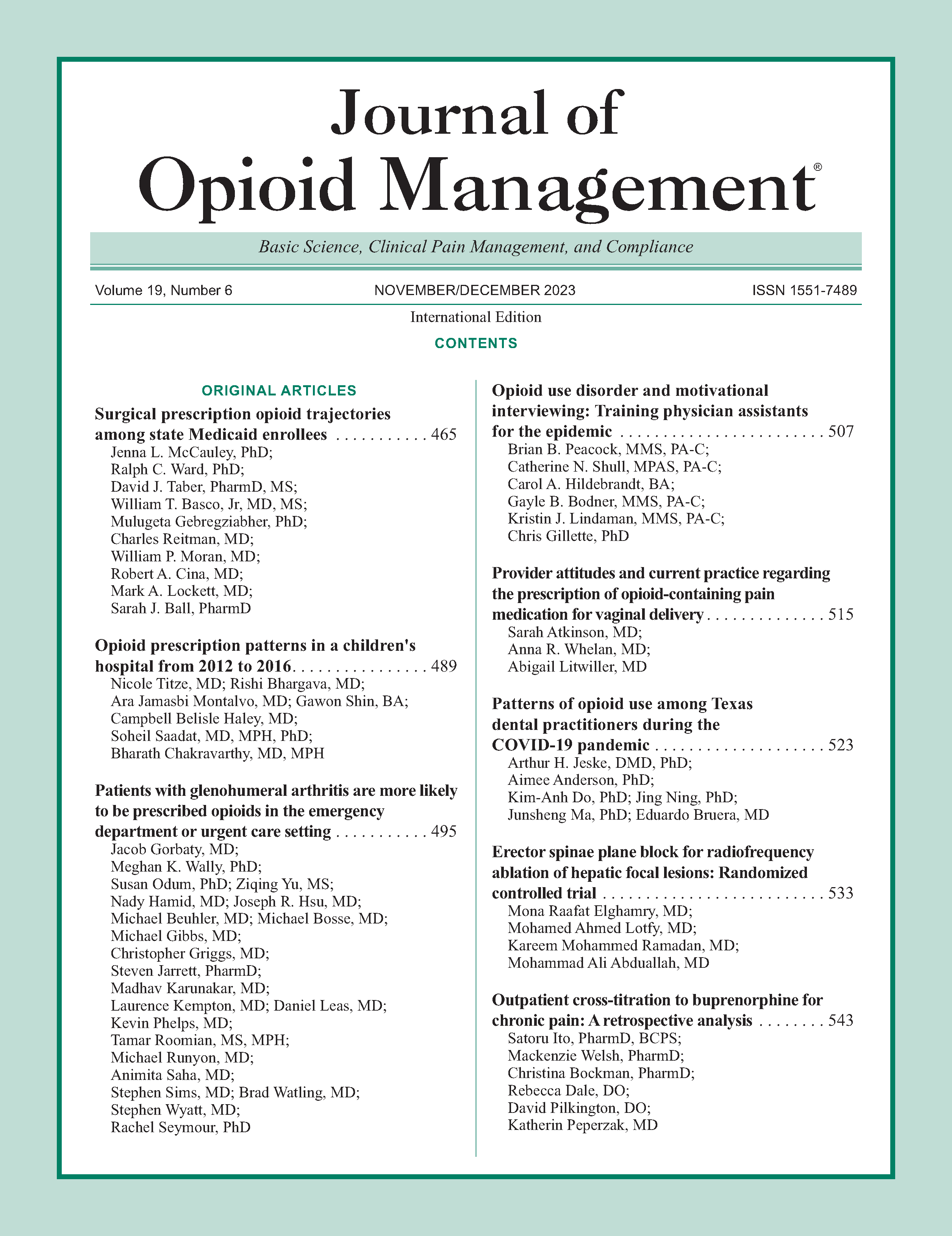
Patients with glenohumeral arthritis are more likely to be prescribed opioids in the emergency department or urgent care setting
DOI:
https://doi.org/10.5055/jom.0834Keywords:
arthritis, decision support, opioids, nonoperative, painAbstract
Objective: The objective is to quantify the rate of opioid and benzodiazepine prescribing for the diagnosis of shoulder osteoarthritis across a large healthcare system and to describe the impact of a clinical decision support intervention on prescribing patterns.
Design: A prospective observational study.
Setting: One large healthcare system.
Patients and participants: Adult patients presenting with shoulder osteoarthritis.
Interventions: A clinical decision support intervention that presents an alert to prescribers when patients meet criteria for increased risk of opioid use disorder.
Main outcome measure: The percentage of patients receiving an opioid or benzodiazepine, the percentage who had at least one risk factor for misuse, and the percent of encounters in which the prescribing decision was influenced by the alert were the main outcome measures.
Results: A total of 5,380 outpatient encounters with a diagnosis of shoulder osteoarthritis were included. Twenty-nine percent (n = 1,548) of these encounters resulted in an opioid or benzodiazepine prescription. One-third of those who received a prescription had at least one risk factor for prescription misuse. Patients were more likely to receive opioids from the emergency department or urgent care facilities (40 percent of encounters) compared to outpatient facilities (28 percent) (p < .0001). Forty-four percent of the opioid prescriptions were for “potent opioids” (morphine milliequivalent conversion factor > 1). Of the 612 encounters triggering an alert, the prescribing decision was influenced (modified or not prescribed) in 53 encounters (8.7 percent). All but four (0.65 percent) of these encounters resulted in an opioid prescription.
Conclusion: Despite evidence against routine opioid use for osteoarthritis, one-third of patients with a primary diagnosis of glenohumeral osteoarthritis received an opioid prescription. Of those who received a prescription, over one-third had a risk factor for opioid misuse. An electronic clinic decision support tool influenced the prescription in less than 10 percent of encounters.
References
Aldington D, Eccleston C: Evidence-based pain management: Building on the foundations of cochrane systematic reviews. Am J Public Health. 2019; 109(1): 46-49. DOI: https://doi.org/10.2105/AJPH.2018.304745
Buckwalter JA, Saltzman C, Brown T: The impact of osteoarthritis: Implications for research. Clin Orthop Relat Res. 2004; (427 Suppl.): S6-S15. DOI: https://doi.org/10.1097/01.blo.0000143938.30681.9d
Oh JH, Chung SW, Oh CH, et al.: The prevalence of shoulder osteoarthritis in the elderly Korean population: Association with risk factors and function. J Shoulder Elbow Surg. 2011; 20(5): 756-763. DOI: https://doi.org/10.1016/j.jse.2011.01.021
van Schaardenburg D, Van den Brande KJ, Ligthart GJ, et al.: Musculoskeletal disorders and disability in persons aged 85 and over: A community survey. Ann Rheum Dis. 1994; 53(12): 807-811. DOI: https://doi.org/10.1136/ard.53.12.807
Luime JJ, Koes BW, Hendriksen IJ, et al.: Prevalence and incidence of shoulder pain in the general population: A systematic review. Scand J Rheumatol. 2004; 33(2): 73-81. DOI: https://doi.org/10.1080/03009740310004667
Smalley CM, Willner MA, Muir MR, et al.: Electronic medical record-based interventions to encourage opioid prescribing best practices in the emergency department. Am J Emerg Med. 2020; 38(8): 1647-1651. DOI: https://doi.org/10.1016/j.ajem.2019.158500
van der Windt DA, Koes BW, de Jong BA, et al.: Shoulder disorders in general practice: Incidence, patient characteristics, and management. Ann Rheum Dis. 1995; 54(12): 959-964. DOI: https://doi.org/10.1136/ard.54.12.959
Huang AR, Mallet L, Rochefort CM, et al.: Medication-related falls in the elderly: Causative factors and preventive strategies. Drugs Aging. 2012; 29(5): 359-376. DOI: https://doi.org/10.2165/11599460-000000000-00000
Hunold KM, Esserman DA, Isaacs CG, et al.: Side effects from oral opioids in older adults during the first week of treatment for acute musculoskeletal pain. Acad Emerg Med. 2013; 20(9): 872-879. DOI: https://doi.org/10.1111/acem.12212
Huang AR, Mallet L: Prescribing opioids in older people. Maturitas. 2013; 74(2): 123-129. DOI: https://doi.org/10.1016/j.maturitas.2012.11.002
AAOS: AAOS releases new clinical practice guideline for osteoarthritis of the hip. 2017.
Chatha K, Borroto W, Goss L, et al.: How orthopedic surgeons can impact opioid use and dependence in shoulder arthroplasty. JSES Int. 2020; 4(1): 105-108. DOI: https://doi.org/10.1016/j.jses.2019.10.113
AAOS: Management of glenohumeral joint osteoarthritis. 2020.
Cheah JW, Sing DC, McLaughlin D, et al.: The perioperative effects of chronic preoperative opioid use on shoulder arthroplasty outcomes. J Shoulder Elbow Surg. 2017; 26(11): 1908-1914. DOI: https://doi.org/10.1016/j.jse.2017.05.016
Lee D, Armaghani S, Archer KR, et al.: Preoperative opioid use as a predictor of adverse postoperative self-reported outcomes in patients undergoing spine surgery. J Bone Joint Surg. 2014; 96(11): e89. DOI: https://doi.org/10.2106/JBJS.M.00865
Weick J, Bawa H, Dirschl DR, et al.: Preoperative opioid use is associated with higher readmission and revision rates in total knee and total hip arthroplasty. J Bone Joint Surg. 2018; 100(14): 1171-1176. DOI: https://doi.org/10.2106/JBJS.17.01414
Thompson KM, Hallock JD, Smith RA, et al.: Preoperative narcotic use and inferior outcomes after anatomic total shoulder arthroplasty: A clinical and radiographic analysis. J Am Acad Orthop Surg. 2019; 27(5): 177-182. DOI: https://doi.org/10.5435/JAAOS-D-16-00808
Morris BJ, Sciascia AD, Jacobs CA, et al.: Preoperative opioid use associated with worse outcomes after anatomic shoulder arthroplasty. J Shoulder Elbow Surg. 2016; 25(4): 619-623. DOI: https://doi.org/10.1016/j.jse.2015.09.017
Springer BD: Management of the bariatric patient. What are the implications of obesity and total joint arthroplasty: The orthopedic surgeon's perspective? J Arthroplasty. 2019; 34(7s): S30-S32. DOI: https://doi.org/10.1016/j.arth.2018.12.021
Hill MV, Stucke RS, McMahon ML, et al.: An educational intervention decreases opioid prescribing after general surgical operations. Ann Surg. 2018; 267(3): 468-472. DOI: https://doi.org/10.1097/SLA.0000000000002198
Kaafarani HMA, Eid AI, Antonelli DM, et al.: Description and impact of a comprehensive multispecialty multidisciplinary intervention to decrease opioid prescribing in surgery. Ann Surg. 2019; 270(3): 452-462. DOI: https://doi.org/10.1097/SLA.0000000000003462
Alamanda VK, Wally MK, Seymour RB, et al.: Prescription reporting with immediate medication utilization mapping G. Prevalence of opioid and benzodiazepine prescriptions for osteoarthritis. Arthritis Care Res. 2020; 72(8): 1081-1086. DOI: https://doi.org/10.1002/acr.23933
Blevins Peratikos M, Weeks HL, Pisansky AJB, et al.: Effect of preoperative opioid use on adverse outcomes, medical spending, and persistent opioid use following elective total joint arthroplasty in the United States: A large retrospective cohort study of administrative claims data. Pain Med. 2020; 21(3): 521-531. DOI: https://doi.org/10.1093/pm/pnz083
Khazi ZM, Lu Y, Patel BH, et al.: Risk factors for opioid use after total shoulder arthroplasty. J Shoulder Elbow Surg. 2020; 29(2): 235-243. DOI: https://doi.org/10.1016/j.jse.2019.06.020
Seymour RB, Leas D, Wally MK, et al.: Prescription reporting with immediate medication utilization mapping (PRIMUM): Development of an alert to improve narcotic prescribing. BMC Med Inform Decis Mak. 2016; 16: 111. DOI: https://doi.org/10.1186/s12911-016-0352-x
Dowell D, Haegerich TM, Chou R: CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep. 2016; 65(1): 1-49. DOI: https://doi.org/10.15585/mmwr.rr6501e1
Dowell D, Ragan KR, Jones CM, et al.: CDC clinical practice guideline for prescribing opioids for pain—United States, 2022. MMWR Recomm Rep. 2022; 71(3): 1-95. DOI: https://doi.org/10.15585/mmwr.rr7103a1
Price-Haywood EG, Burton J, Burstain T, et al.: Clinical effectiveness of decision support for prescribing opioids for chronic noncancer pain: A prospective cohort study. Value Health. 2020; 23(2): 157-163. DOI: https://doi.org/10.1016/j.jval.2019.09.2748
Rayo MF, Moffatt-Bruce SD: Alarm system management: Evidence-based guidance encouraging direct measurement of informativeness to improve alarm response. BMJ Qual Saf. 2015; 24(4): 282-286. DOI: https://doi.org/10.1136/bmjqs-2014-003373
van der Sijs H, van Gelder T, Vulto A, et al.: Understanding handling of drug safety alerts: A simulation study. Int J Med Inform. 2010; 79(5): 361-369. DOI: https://doi.org/10.1016/j.ijmedinf.2010.01.008
Weingart SN, Toth M, Sands DZ, et al.: Physicians' decisions to override computerized drug alerts in primary care. Arch Intern Med. 2003; 163(21): 2625-2631. DOI: https://doi.org/10.1001/archinte.163.21.2625
van der Sijs H, Aarts J, Vulto A, et al.: Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006; 13(2): 138-147. DOI: https://doi.org/10.1197/jamia.M1809
Ancker JS, Edwards A, Nosal S, et al.: Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. 2017; 17(1): 36. DOI: https://doi.org/10.1186/s12911-017-0430-8
Chiu AS, Jean RA, Hoag JR, et al.: Association of lowering default pill counts in electronic medical record systems with postoperative opioid prescribing. JAMA Surg. 2018; 153(11): 1012-1019. DOI: https://doi.org/10.1001/jamasurg.2018.2083
Meisenberg BR, Grover J, Campbell C, et al.: Assessment of opioid prescribing practices before and after implementation of a health system intervention to reduce opioid overprescribing. JAMA Netw Open. 2018; 1(5): e182908. DOI: https://doi.org/10.1001/jamanetworkopen.2018.2908
Bauer SR, Hitchner L, Harrison H, et al.: Predictors of higher-risk chronic opioid prescriptions in an academic primary care setting. Subst Abus. 2016; 37(1): 110-117. DOI: https://doi.org/10.1080/08897077.2015.1129020
Sudhir Singh SG, Mohammad F, Kumar S, et al.: Prevalence of shoulder disorders in tertiary care Centre. Int J Res Med Sci. 2015; 3(4): 917. DOI: https://doi.org/10.5455/2320-6012.ijrms20150419
McLaughlin DC, Cheah JW, Aleshi P, et al.: Multimodal analgesia decreases opioid consumption after shoulder arthroplasty: A prospective cohort study. J Shoulder Elbow Surg. 2018; 27(4): 686-691. DOI: https://doi.org/10.1016/j.jse.2017.11.015
Bloom DA, Manjunath AK, Gotlin MJ, et al.: Institutional reductions in opioid prescribing do not change patient satisfaction on press Ganey surveys after total shoulder arthroplasty. J Shoulder Elbow Surg. 2021; 30(4): 858-864. DOI: https://doi.org/10.1016/j.jse.2020.07.016
Etcheson JI, Gwam CU, George NE, et al.: Opioids consumed in the immediate post-operative period do not influence how patients rate their experience of care after total hip arthroplasty. J Arthroplasty. 2018; 33(4): 1008-1011. DOI: https://doi.org/10.1016/j.arth.2017.10.033
Leas DP, Connor PM, Schiffern SC, et al.: Opioid-free shoulder arthroplasty: A prospective study of a novel clinical care pathway. J Shoulder Elbow Surg. 2019; 28(9): 1716-1722. DOI: https://doi.org/10.1016/j.jse.2019.01.013
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.