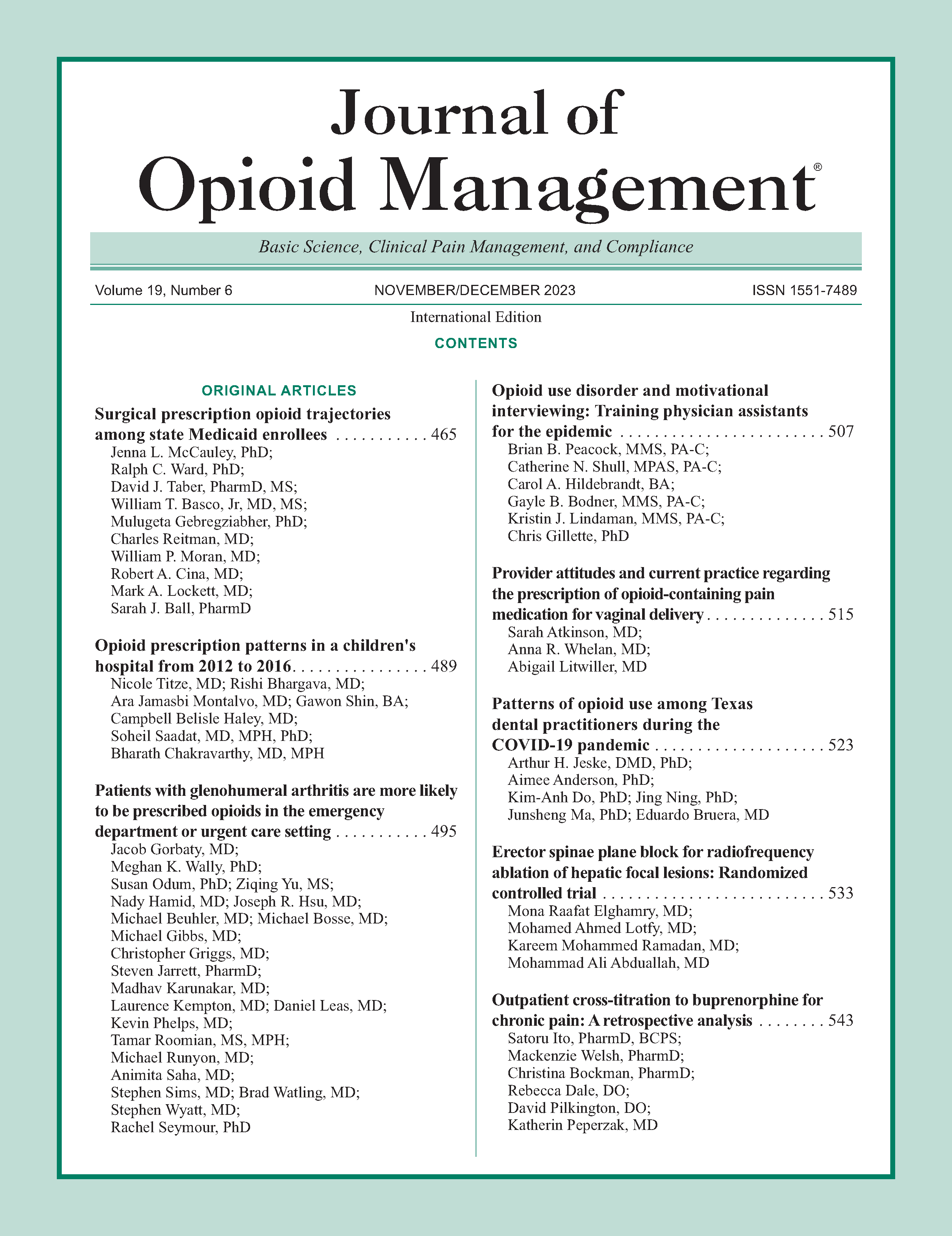
Provider attitudes and current practice regarding the prescription of opioid-containing pain medication for vaginal delivery
DOI:
https://doi.org/10.5055/jom.0836Keywords:
analgesics, opioid, obstetric delivery, opioid abuse, post-partumAbstract
Background: The epidemic of opioid misuse and abuse is rampant in the United States. A large percentage of patients who go on to misuse or abuse opioids were initially legally prescribed an opioid medication by their physician. One of the most common reasons patients of reproductive age seek medical care is for pregnancy and delivery. These patients are frequently prescribed opioids. Greater than one in 10 Medicaid-enrolled women fill an opioid prescription after vaginal delivery.
Objective: To assess the opioid prescribing patterns of obstetric providers following vaginal deliveries.
Study design: Obstetric physicians and certified nurse midwives (CNMs) from different practice backgrounds were administered a questionnaire regarding opioid prescribing practices for patients who undergo vaginal delivery. Providers were contacted via email and completed survey via REDCap.
Results: Ninety-nine providers completed the survey between October 2018 and January 2019. Eight percent of all providers reported prescribing opioids at discharge after vaginal deliveries. There was a statistically significant difference in the proportion of physicians who provided opioid prescriptions at discharge compared to CNMs (16.7 percent vs 1.8 percent, respectively, p < .05). Common reasons for prescribing opioids at discharge included post-partum tubal ligation (56.4 percent), third- and fourth-degree lacerations (59.6 and 73.4 percent, respectively), and operative deliveries (26.6 percent). Physicians were significantly more likely to prescribe an opioid after a second-degree laceration than CNMs (19.1 percent vs 5.3 percent, p < 0.05).
Conclusions: Practice patterns for opioid prescription vary by provider type as well as by delivery characteristics. Further study is necessary to delineate the optimal care while minimizing unnecessary opioid prescriptions.
References
Centers for Disease Control and Prevention: Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011; 60(43): 1487-1492.
Hedegaard H, Minino AM, Warner M: Drug overdose deaths in the United States, 1999-2019. NCHS Data Brief. 2020; 394: 1-8.
Compton WM, Jones CM, Baldwin GT: Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016; 374(2): 154-163. DOI: 10.1056/NEJMra1508490. DOI: https://doi.org/10.1056/NEJMra1508490
Hagemeier NE: Introduction to the opioid epidemic: The economic burden on the healthcare system and impact on quality of life. Am J Manag Care. 2018; 24(10 Suppl.): S200-S206.
Olsen Y: The CDC guideline on opioid prescribing: Rising to the challenge. JAMA. 2016; 315(15): 1577-1579. DOI: 10.1001/jama.2016.1910. DOI: https://doi.org/10.1001/jama.2016.1910
Osmundson SS, Min JY, Grijalva CG: Opioid prescribing after childbirth: Overprescribing and chronic use. Curr Opin Obstet Gynecol. 2019; 31(2): 83-89. DOI: 10.1097/GCO.0000000000000527. DOI: https://doi.org/10.1097/GCO.0000000000000527
Manchikanti L, Abdi S, Atluri S, et al.: American society of interventional pain physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2–guidance. Pain Phys. 2012; 15(3 Suppl.): S67-S116. DOI: https://doi.org/10.36076/ppj.2012/15/S67
American College of Obstetricians and Gynecologists' Committee on Clinical Consensus–Obstetrics: Pharmacologic stepwise multimodal approach for postpartum pain management: ACOG clinical consensus no. 1. Obstet Gynecol. 2021; 138(3): 507-517. DOI: 10.1097/AOG.0000000000004517. DOI: https://doi.org/10.1097/AOG.0000000000004517
Baruch AD, Morgan DM, Dalton VK, et al.: Opioid prescribing patterns by obstetrics and gynecology residents in the United States. Subst Use Misuse. 2018; 53(1): 70-76. DOI: 10.1080/10826084.2017.1323928. DOI: https://doi.org/10.1080/10826084.2017.1323928
Bateman BT, Cole NM, Maeda A, et al.: Patterns of opioid prescription and use after cesarean delivery. Obstet Gynecol. 2017; 130(1): 29-35. DOI: 10.1097/AOG.0000000000002093. DOI: https://doi.org/10.1097/AOG.0000000000002093
Jarlenski M, Bodnar LM, Kim JY, et al.: Filled prescriptions for opioids after vaginal delivery. Obstet Gynecol. 2017; 129(3): 431-437. DOI: 10.1097/AOG.0000000000001868. DOI: https://doi.org/10.1097/AOG.0000000000001868
Ko JY, D'Angelo DV, Haight SC, et al.: Vital signs: Prescription opioid pain reliever use during pregnancy—34 US Jurisdictions, 2019. MMWR Morb Mortal Wkly Rep. 2020; 69(28): 897-903. DOI: 10.15585/mmwr.mm6928a1. DOI: https://doi.org/10.15585/mmwr.mm6928a1
Prabhu M, McQuaid-Hanson E, Hopp S, et al.: A shared decision-making intervention to guide opioid prescribing after cesarean delivery. Obstet Gynecol. 2017; 130(1): 42-46. DOI: 10.1097/AOG.0000000000002094. DOI: https://doi.org/10.1097/AOG.0000000000002094
ACOG Committee Opinion No. 742: Postpartum pain management. Obstet Gynecol. 2018; 132(1): e35-e43. DOI: 10.1097/AOG.0000000000002683. DOI: https://doi.org/10.1097/AOG.0000000000002683
Mourad M, Landau R, Wright JD, et al.: Oral opioid use during vaginal delivery hospitalizations. Am J Perinatol. 2020; 37(4): 390-397. DOI: 10.1055/s-0039-1678566. DOI: https://doi.org/10.1055/s-0039-1678566
Harris PA, Taylor R, Thielke R, et al.: Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42(2): 377-381. DOI: 10.1016/j.jbi.2008.08.010. DOI: https://doi.org/10.1016/j.jbi.2008.08.010
Mack KA, Zhang K, Paulozzi L, et al.: Prescription practices involving opioid analgesics among Americans with Medicaid, 2010. J Health Care Poor Underserved. 2015; 26(1): 182-198. DOI: 10.1353/hpu.2015.0009. DOI: https://doi.org/10.1353/hpu.2015.0009
Yang YT, Attanasio LB, Kozhimannil KB: State scope of practice laws, nurse-midwifery workforce, and childbirth procedures and outcomes. Womens Health Issues. 2016; 26(3): 262-267. DOI: 10.1016/j.whi.2016.02.003. DOI: https://doi.org/10.1016/j.whi.2016.02.003
Badreldin N, Grobman WA, Chang KT, et al.: Opioid prescribing patterns among postpartum women. Am J Obstet Gynecol. 2018; 219(1): 103e1–103-e8. DOI: 10.1016/j.ajog.2018.04.003. DOI: https://doi.org/10.1016/j.ajog.2018.04.003
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.