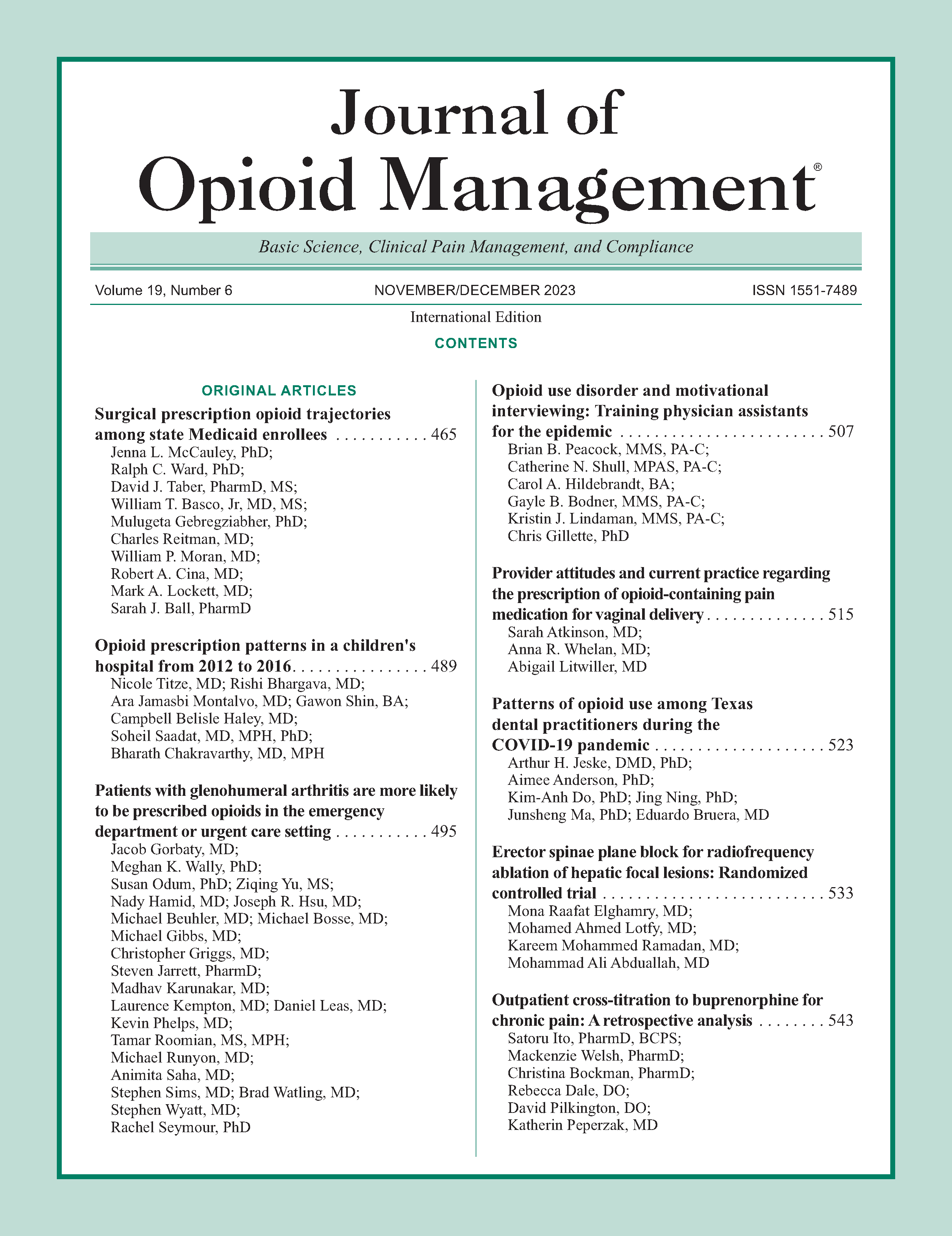
Erector spinae plane block for radiofrequency ablation of hepatic focal lesions: Randomized controlled trial
DOI:
https://doi.org/10.5055/jom.0838Keywords:
conscious sedation, erector spinae plane block, fentanyl, liver neoplasms, radiofrequency ablationAbstract
Objective: This study evaluated the opioid sparing and pain relief effect of erector spinae plane block (ESPB) for radiofrequency ablation (RFA) of hepatic focal lesions under conscious sedation.
Design: A randomized controlled trial.
Setting: Tanta University Hospitals.
Patients: Fifty patients aged 30-60 years old and eligible for RFA of hepatic focal lesions were included.
Interventions: Patients randomized to receive either local anesthetic infiltration (group I) or ESPB (group II). Both groups received sedation by propofol infusion.
Main outcome measure(s): The primary outcome was total fentanyl consumption. Secondary outcomes were nonverbal pain score (NVPS), time to first analgesic request post-procedure, radiologist's satisfaction, and complications.
Results: In group I, NVPS was significantly increased at 10, 15, 25, and 30 minutes during RFA compared to group II (p = 0.008, <0.001, 0.018, and 0.001, respectively) with no significant differences on arrival to post-anesthesia care unit (PACU) and after 1 hour. Total fentanyl consumption during the procedure was significantly increased in group I compared to group II (160.9 ± 38.2 and 76 ± 21 μg, respectively; p < 0.001) with prolonged time to first analgesia request post-procedure in group II compared to group I (392.7 ± 38.8 and 101.1 ± 13.6 minutes, respectively; p < 0.001). The level of radiologist's satisfaction was significantly increased in the group II (p = 0.010). Three patients in group I and one patient in group II needed general anesthesia. Lower incidence of complications in group II occurred with statistical insignificance.
Conclusions: The ESPB provided adequate analgesia and reduced opioids consumption during the hepatic RFA, with high radiologist's satisfaction.
References
Amornyotin S, Jirachaipitak S, Wangnatip S: Anesthetic management for radiofrequency ablation in patients with hepatocellular carcinoma in a developing country. J Anesth Crit Care. 2015; 3(1): 00086. DOI: 10.15406/jaccoa.2015.03.00086. DOI: https://doi.org/10.15406/jaccoa.2015.03.00086
Chakravorty N, Jaiswal S, Chakravarty D, et al.: Anaesthetic management of radiofrequency tumor ablation: Our experience. Indian J Anaesth. 2006; 50(2): 123-127. DOI: 10.4103/joacp.JOACP_39_17. DOI: https://doi.org/10.4103/joacp.JOACP_39_17
Piccioni F, Fumagalli L, Garbagnati F, et al.: Thoracic paravertebral anesthesia for percutaneous radiofrequency ablation of hepatic tumors. J Clin Anesth. 2014; 26(4): 271-275. DOI: 10.1016/j.jclinane.2013.11.019. DOI: https://doi.org/10.1016/j.jclinane.2013.11.019
Chin K, Adhikary S, Sarwani N, et al.: The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017; 72(4): 452-460. DOI: 10.1111/anae.13814. DOI: https://doi.org/10.1111/anae.13814
Chin KJ, Malhas L, Perlas A: The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: A report of 3 cases. Reg Anesth Pain Med. 2017; 42(3): 372-376. DOI: 10.1097/AAP.0000000000000581. DOI: https://doi.org/10.1097/AAP.0000000000000581
Tulgar S, Selvi O, Senturk O, et al.: Ultrasound-guided erector spinae plane block: Indications, complications, and effects on acute and chronic pain based on a single-center experience. Cureus. 2019; 11(1): e3815. DOI: 10.7759/cureus.3815. DOI: https://doi.org/10.7759/cureus.3815
Pereira-Morales S, Arroyo-Novoa CM, Wysocki A, et al.: Acute pain assessment in sedated patients in the postanesthesia care unit. Clin J Pain. 2018; 34(8): 700-706. DOI: 10.1097/AJP.0000000000000593. DOI: https://doi.org/10.1097/AJP.0000000000000593
Marmo L, Fowler S: Pain assessment tool in the critically ill post–open heart surgery patient population. Pain Manag Nurs. 2010; 11(3): 134-140. DOI: 10.1016/j.pmn.2009.05.007. DOI: https://doi.org/10.1016/j.pmn.2009.05.007
Guay J, Nishimori M, Kopp SL: Epidural local anesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting, and pain after abdominal surgery: A Cochrane review. Anesth Analg. 2016; 123(6): 1591-1602. DOI: 10.1213/ANE.0000000000001628. DOI: https://doi.org/10.1213/ANE.0000000000001628
Rawal N: Epidural technique for postoperative pain: Gold standard no more? Reg Anesth Pain Med. 2012; 37(3): 310-317. DOI: 10.1097/AAP.0b013e31825735c6. DOI: https://doi.org/10.1097/AAP.0b013e31825735c6
Niraj G, Kelkar A, Hart E, et al.: Four quadrant transversus abdominis plane block and continuous transversus abdominis plane analgesia: A 3-year prospective audit in 124 patients. J Clin Anesth. 2015; 27(7): 579-584. DOI: 10.1016/j.jclinane.2015.07.005. DOI: https://doi.org/10.1016/j.jclinane.2015.07.005
Ganapathy S, Sondekoppam RV, Terlecki M, et al.: Comparison of efficacy and safety of lateral-to-medial continuous transversus abdominis plane block with thoracic epidural analgesia in patients undergoing abdominal surgery: A randomised, open-label feasibility study. Eur J Anaesthesiol. 2015; 32(11): 797-804. DOI: 10.1097/EJA.0000000000000345. DOI: https://doi.org/10.1097/EJA.0000000000000345
Chin KJ, McDonnell JG, Carvalho B, et al.: Essentials of our current understanding: Abdominal wall blocks. Reg Anesth Pain Med. 2017; 42(2): 133-183. DOI: 10.1097/AAP.0000000000000545. DOI: https://doi.org/10.1097/AAP.0000000000000545
Baeriswyl M, Kirkham KR, Kern C, et al.: The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: A meta-analysis. Anesth Analg. 2015; 121(6): 1640-1654. DOI: 10.1213/ANE.0000000000000967. DOI: https://doi.org/10.1213/ANE.0000000000000967
Bang S, Chung J, Kwon W, et al.: Erector spinae plane block for multimodal analgesia after wide midline laparotomy: A case report. Medicine. 2019; 98(20): e15654. DOI: 10.1097/MD.0000000000015654. DOI: https://doi.org/10.1097/MD.0000000000015654
Hamed MA, Goda AS, Basiony MM, et al.: Erector spinae plane block for postoperative analgesia in patients undergoing total abdominal hysterectomy: A randomized controlled study original study. J Pain Res. 2019; 12: 1393-1398. DOI: 10.2147/JPR.S196501. DOI: https://doi.org/10.2147/JPR.S196501
Luis-Navarro JC, Seda-Guzmán M, Luis-Moreno C, et al.: Erector spinae plane block in abdominal surgery: Case series. Indian J Anaesth. 2018; 62(7): 549-554. DOI: 10.4103/ija.IJA_57_18. DOI: https://doi.org/10.4103/ija.IJA_57_18
Petsas D, Pogiatzi V, Galatidis T, et al.: Erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: A case report. J Pain Res. 2018; 11: 1983-1990. DOI: 10.1111/papr.12953. DOI: https://doi.org/10.2147/JPR.S164489
Tulgar S, Kapakli MS, Senturk O, et al.: Evaluation of ultrasound- guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: A prospective, randomized, controlled clinical trial. J Clin Anesth. 2018; 49: 101-106. DOI: 10.1016/j.jclinane.2018.06.019. DOI: https://doi.org/10.1016/j.jclinane.2018.06.019
De Cassai A, Bonvicini D, Correale C, et al.: Erector spinae plane block: A systematic qualitative review. Minerva Anestesiol. 2019; 85(3): 308-319. DOI: 10.23736/s0375-9393.18.13341-4. DOI: https://doi.org/10.23736/S0375-9393.18.13341-4
Aponte A, Sala-Blanch X, Prats-Galino A, et al.: Anatomical evaluation of the extent of spread in the erector spinae plane block: A cadaveric study. Can J Anesth/J Can Anesth. 2019; 66(8): 886-893. DOI: 10.1007/s12630-019-01399-4. DOI: https://doi.org/10.1007/s12630-019-01399-4
Tulgar S, Kapakli MS, Kose HC, et al.: Evaluation of ultrasound- guided erector spinae plane block and oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy: Randomized, controlled, prospective study. Anesth Essays Res. 2019; 13(1): 50-56. DOI: 10.4103/aer.AER_194_18. DOI: https://doi.org/10.4103/aer.AER_194_18
Kang R, Chin KJ, Gwak MS, et al.: Bilateral single-injection erector spinae plane block versus intrathecal morphine for postoperative analgesia in living donor laparoscopic hepatectomy: A randomized non-inferiority trial. Reg Anesth Pain Med. 2019; 44(12): rapm-2019-100902-1065. DOI: 10.1136/rapm-2019-100902. DOI: https://doi.org/10.1136/rapm-2019-100902
Hacibeyoglu G, Topal A, Arican S, et al.: USG guided bilateral erector spinae plane block is an effective and safe postoperative analgesia method for living donor liver transplantation. J Clin Anesth. 2018; 49: 36-37. DOI: 10.1016/j.jclinane.2018.06.003. DOI: https://doi.org/10.1016/j.jclinane.2018.06.003
Moore RP, Liu C-J, George P, et al.: Early experiences with the use of continuous erector spinae plane blockade for the provision of perioperative analgesia for pediatric liver transplant recipients. Reg Anesth Pain Med. 2019; 44(6): 679-682. DOI: 10.1136/rapm-2018-100253. DOI: https://doi.org/10.1136/rapm-2018-100253
Elkoundi A, Eloukkal Z, Bensghir M, et al.: Erector spinae plane block for hyperalgesic acute pancreatitis. Pain Med. 2019; 20(5): 1055-1056. DOI: 10.1093/pm/pny232. DOI: https://doi.org/10.1093/pm/pny232
Kose HC, Kose SG, Thomas DT: Lumbar versus thoracic erector spinae plane block: Similar nomenclature, different mechanism of action. J Clin Anesth. 2018; 48: 1. DOI: 10.1016/j.jclinane.2018.03.026. DOI: https://doi.org/10.1016/j.jclinane.2018.03.026
Forero M, Adhikary SD, Lopez H, et al.: The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016; 41(5): 621-627. DOI: 10.1097/AAP.0000000000000451. DOI: https://doi.org/10.1097/AAP.0000000000000451
De Cassi A, Tonetti T: Local anesthetic spread during erector spinae plane block. J Clin Anesth. 2018; 48: 60-61. DOI: 10.1016/j.jclinane.2018.05.003. DOI: https://doi.org/10.1016/j.jclinane.2018.05.003
Nagaraja P, Ragavendran S, Singh NG, et al.: Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann Card Anaesth. 2018; 21(3): 323-327. DOI: 10.4103/aca.ACA_16_18. DOI: https://doi.org/10.4103/aca.ACA_16_18
Hamilton DL: Pneumothorax following erector spinae plane block. J Clin Anesth. 2019; 52: 17. DOI: 10.1016/j.jclinane.2018.08.026. DOI: https://doi.org/10.1016/j.jclinane.2018.08.026
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.