Appendix: The effects of physician stigma and hesitancy with opioids on patient pain care in the United States: A survey study
DOI:
https://doi.org/10.5055/jom.0872-AppendixKeywords:
survey, physician stigma, opioids, opioid use disorder, substance use disorder, chronic pain, pain medicineAbstract
Objectives: Determine if physician stigma toward patients with chronic pain or opioid use disorder or physician hesitancy prescribing opioids adversely affects patient pain care. Explore the demographics associated with stigma and hesitancy.
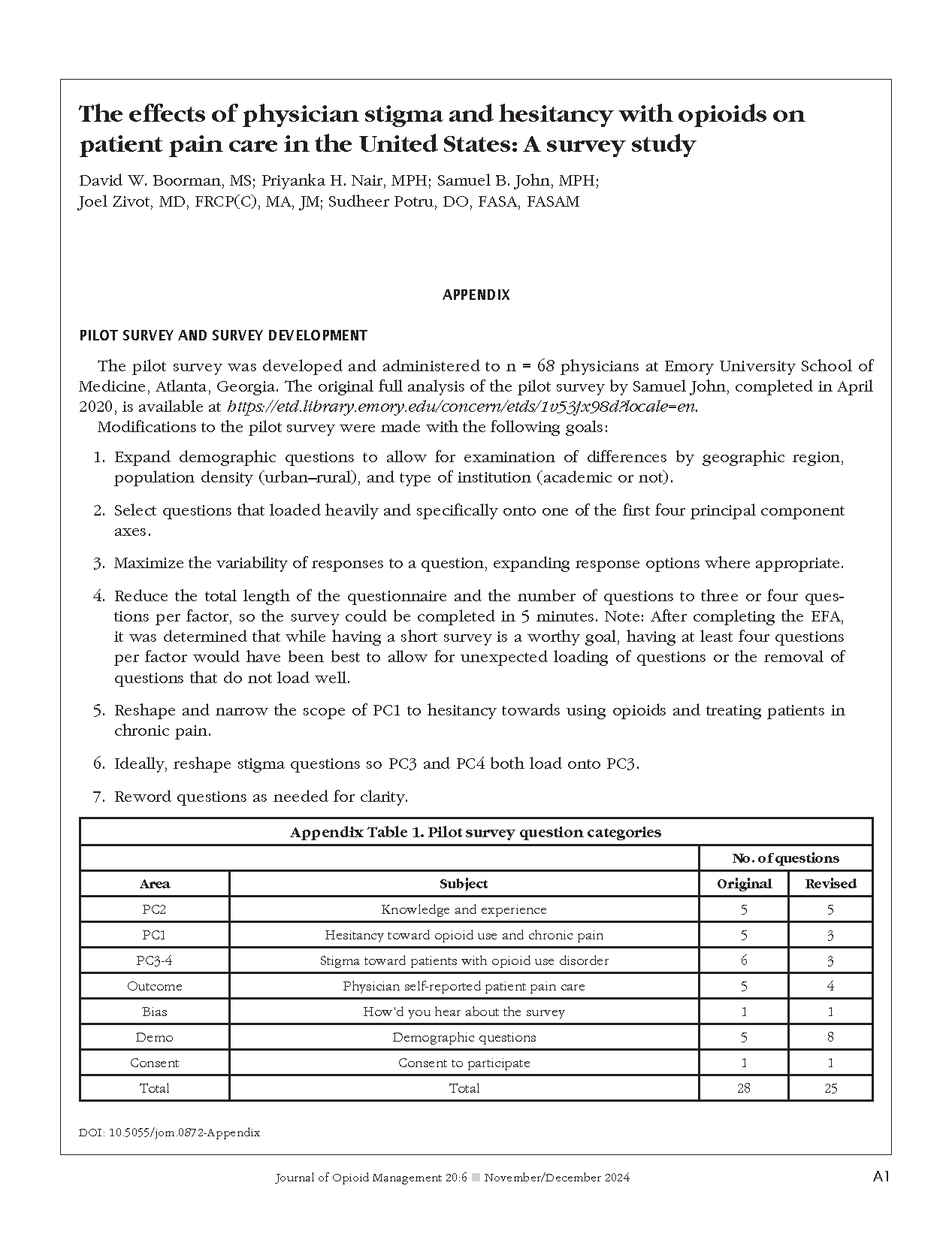
Design: Survey, 25 questions.
Setting: Physician faculty at medical schools (80 percent), private physician Facebook® groups (15 percent), and others (5 percent), all specialties.
Participants: N = 352 attending United States physicians.
Main outcome measure: Physician self-reported patient pain care quality.
Results: Subjectively worse patient pain care was not found to be associated with stigma but had a borderline association with hesitancy (p = 0.046). Subjectively worse pain care was associated with less knowledge and experience with opioids (odds ratio [OR] 4.1, 95 percent confidence interval [CI] 3.0-5.6), practicing in the Midwest region (OR 2.1, 95 percent CI 1.2-3.4), and specialty: emergency (OR 53, 95 percent CI 20-139), other internal (OR 15, 95 percent CI 6.6-34), and general medicine (OR 12, 95 percent CI 5.4-26) compared to pain medicine. Physician stigma was more likely to be high in males (OR 2.5, 95 percent CI 1.5-4.3) and medium in physicians over 55 (OR 2.5, 95 percent CI 1.5-4.5). Compared to medium stigma, those with low stigma (General Linear Model (GLM) 0.35, 95 percent CI 0.18-0.52) and high stigma (GLM 0.22, 95 percent CI 0.01-0.44) were both more hesitant to prescribe opioids. More hesitancy was associated with less knowledge and experience (GLM 0.14, 95 percent CI 0.05-0.22) and physicians under 55 (GLM 0.24, 95 percent CI 0.08-0.40).
Conclusions: Although physician stigma was not found to affect patient pain care adversely, self-reporting bias and/or questionnaire issues may account for this. Physician specialty and knowledge and experience with opioids were important factors.
References
Dayer LE, Painter JT, McCain K, et al.: A recent history of opioid use in the US: Three decades of change. Subst Use Misuse. 2019; 54(2): 331-339. DOI: 10.1080/10826084.2018.1517175. DOI: https://doi.org/10.1080/10826084.2018.1517175
Centers for Disease Control and Prevention: Understanding the opioid overdose epidemic. Available at https://www.cdc.gov/opioids/basics/epidemic.html. Accessed September 25, 2023.
Owens B: Opioid prescriptions down but some patients fear doctors now too strict. CMAJ. 2019; 191(19): E546-E547. DOI: 10.1503/cmaj.109-5748. DOI: https://doi.org/10.1503/cmaj.109-5748
Kroenke K, Alford DP, Argoff C, et al.: Challenges with implementing the centers for disease control and prevention opioid guideline: A consensus panel report. Pain Med. 2019; 20(4): 724-735. DOI: 10.1093/pm/pny307. DOI: https://doi.org/10.1093/pm/pny307
O'Brien JB, Roman DL: Novel treatments for chronic pain: Moving beyond opioids. Transl Res. 2021; 234: 1-19. DOI: 10.1016/j.trsl.2021.03.008. DOI: https://doi.org/10.1016/j.trsl.2021.03.008
Dineen KK, DuBois JM: Between a rock and a hard place: Can physicians prescribe opioids to treat pain adequately while avoiding legal sanction? Am J Law Med. 2016; 42(1): 7-52. DOI: 10.1177/0098858816644712. DOI: https://doi.org/10.1177/0098858816644712
Heimer R, Hawk K, Vermund SH: Prevalent misconceptions about opioid use disorders in the United States produce failed policy and public health responses. Clin Infect Dis. 2019; 69(3): 546-551. DOI: 10.1093/cid/ciy977. DOI: https://doi.org/10.1093/cid/ciy977
American Medical Association: Report shows decreases in opioid prescribing, increase in overdoses. Available at https://www.ama-assn.org/press-center/press-releases/report-showsdecreases-opioid-prescribing-increase-overdoses. Accessed September 21, 2021.
Busse JW, Juurlink D, Guyatt GH: Addressing the limitations of the CDC guideline for prescribing opioids for chronic noncancer pain. CMAJ. 2016; 188(17-18): 1210-1211. DOI: 10.1503/cmaj.161023. DOI: https://doi.org/10.1503/cmaj.161023
Garpenhag L, Dahlman D: Perceived healthcare stigma among patients in opioid substitution treatment: A qualitative study. Subst Abuse Treat Prev Policy. 2021; 16(1): 81. DOI: 10.1186/s13011-021-00417-3. DOI: https://doi.org/10.1186/s13011-021-00417-3
McCurry MK, Avery-Desmarais S, Schuler M, et al.: Perceived stigma, barriers, and facilitators experienced by members of the opioid use disorder community when seeking healthcare. J Nurs Scholarsh. 2023; 55(3): 701-710. DOI: 10.1111/jnu.12837. DOI: https://doi.org/10.1111/jnu.12837
Dhanani LY, Franz B, Hall TK: Revisiting the relationship between contact and physician attitudes toward patients with opioid use disorder. Addict Behav Rep. 2021; 14: 100372. DOI: 10.1016/j.abrep.2021.100372. DOI: https://doi.org/10.1016/j.abrep.2021.100372
Stone EM, Kennedy-Hendricks A, Barry CL, et al.: The role of stigma in US primary care physicians' treatment of opioid use disorder. Drug Alcohol Depend. 2021; 221: 108627. DOI: 10.1016/j.drugalcdep.2021.108627. DOI: https://doi.org/10.1016/j.drugalcdep.2021.108627
Mendiola CK, Galetto G, Fingerhood M: An exploration of emergency physicians' attitudes toward patients with substance use disorder. J Addict Med. 2018; 12(2): 132-135. DOI: 10.1097/ADM.0000000000000377. DOI: https://doi.org/10.1097/ADM.0000000000000377
Louie DL, Assefa MT, McGovern MP: Attitudes of primary care physicians toward prescribing buprenorphine: A narrative review. BMC Fam Pract. 2019; 20(1): 157. DOI: 10.1186/s12875-019-1047-z. DOI: https://doi.org/10.1186/s12875-019-1047-z
van Boekel LC, Brouwers EP, van Weeghel J, et al.: Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int J Soc Psychiatry. 2015; 61(6): 539-549. DOI: 10.1177/0020764014562051. DOI: https://doi.org/10.1177/0020764014562051
Andraka-Christou B, Capone MJ: A qualitative study comparing physician-reported barriers to treating addiction using buprenorphine and extended-release naltrexone in US office-based practices. Int J Drug Policy. 2018; 54: 9-17. DOI: 10.1016/j.drugpo.2017.11.021. DOI: https://doi.org/10.1016/j.drugpo.2017.11.021
John S, Boorman DW, Potru S: Identifying barriers to buprenorphine treatment for patients with opioid use disorder among anesthesiologists and pain practitioners: A survey study. J Addict Med. 2023; 17(2): e94-e100. DOI: 10.1097/ADM.0000000000001066. DOI: https://doi.org/10.1097/ADM.0000000000001066
Shreffler J, Shaw I, McGee S, et al.: Perceptions diverge on aspects related to substance use disorder: An analysis of individuals in recovery, physicians, nurses, and medical students. Subst Abus. 2021; 42(4): 896-904. DOI: 10.1080/08897077.2021.1892014. DOI: https://doi.org/10.1080/08897077.2021.1892014
Dubin RE, Kaplan A, Graves L, et al.: Acknowledging stigma: Its presence in patient care and medical education. Can Fam Physician. 2017; 63(12): 906-908.
Adams JM, Volkow ND: Ethical imperatives to overcome stigma against people with substance use disorders. AMA J Ethics. 2020; 22(1): E702-E708. DOI: 10.1001/amajethics.2020.702. DOI: https://doi.org/10.1001/amajethics.2020.702
Dassieu L, Heino A, Develay E, et al.: “They think you're trying to get the drug”: Qualitative investigation of chronic pain patients' health care experiences during the opioid overdose epidemic in Canada. Can J Pain. 2021; 5(1): 66-80. DOI: 10.1080/24740527.2021.1881886. DOI: https://doi.org/10.1080/24740527.2021.1881886
Cohen M, Quintner J, Buchanan D, et al.: Stigmatization of patients with chronic pain: The extinction of empathy. Pain Med. 2011; 12(11): 1637-1643. DOI: 10.1111/j.1526-4637.2011.01264.x. DOI: https://doi.org/10.1111/j.1526-4637.2011.01264.x
Roche J, Harmon D: Exploring the facets of empathy and pain in clinical practice: A review. Pain Pract. 2017; 17(8): 1089-1096. DOI: 10.1111/papr.12563. DOI: https://doi.org/10.1111/papr.12563
Huang CJ: On being the “right” kind of chronic pain patient. Narrat Inq Bioeth. 2018; 8(3): 239-245. DOI: 10.1353/nib.2018.0073. DOI: https://doi.org/10.1353/nib.2018.0073
Battin SG, Romsland GI, Christiansen B: Diminishing pain stigma: Patient perceptions of encounters with interprofessional teams in biopsychosocial pain rehabilitation. Ann Med. 2022; 54(1): 2561-2572. DOI: 10.1080/07853890.2022.2124447. DOI: https://doi.org/10.1080/07853890.2022.2124447
Goldberg DS: Pain, objectivity and history: Understanding pain stigma. Med Humanit. 2017; 43(4): 238-243. DOI: 10.1136/medhum-2016-011133. DOI: https://doi.org/10.1136/medhum-2016-011133
McCradden MD, Vasileva D, Orchanian-Cheff A, et al.: Ambiguous identities of drugs and people: A scoping review of opioid-related stigma. Int J Drug Policy. 2019; 74: 205-215. DOI: 10.1016/j.drugpo.2019.10.005. DOI: https://doi.org/10.1016/j.drugpo.2019.10.005
Kreek MJ, Reed B, Butelman ER: Current status of opioid addiction treatment and related preclinical research. Sci Adv. 2019; 5(10): eaax9140. DOI: 10.1126/sciadv.aax9140. DOI: https://doi.org/10.1126/sciadv.aax9140
Perugino F, De Angelis V, Pompili M, et al.: Stigma and chronic pain. Pain Ther. 2022; 11(4): 1085-1094. DOI: 10.1007/s40122-022-00418-5. DOI: https://doi.org/10.1007/s40122-022-00418-5
Sedney CL, Dekeseredy P, Singh SA, et al.: Stigmatizing language expressed towards individuals with current or previous OUD who have pain and cancer: A qualitative study. J Pain Symptom Manage. 2023; 65(6): 553-561. DOI: 10.1016/j.jpainsymman.2023.02.007. DOI: https://doi.org/10.1016/j.jpainsymman.2023.02.007
Singh SA, Moreland RA, Fang W, et al.: Compassion inequities and opioid use disorder: A matched case–control analysis examining inpatient management of cancer-related pain for patients with opioid use disorder. J Pain Symptom Manage. 2021; 62(3): e156-e163. DOI: 10.1016/j.jpainsymman.2021.05.002. DOI: https://doi.org/10.1016/j.jpainsymman.2021.05.002
John S: Physician Attitudes and Stigma May Hinder Patient Care with Opioid Prescribing, Pain Management, and Addiction Treatment. Atlanta, GA: Emory University, 2020. Available at https://etd.library.emory.edu/concern/etds/1v53jx98d?locale=en. Accessed September 25, 2023.
Harris PA, Taylor R, Thielke R, et al.: Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42(2): 377-381. DOI: 10.1016/j.jbi.2008.08.010. DOI: https://doi.org/10.1016/j.jbi.2008.08.010
Harris PA, Taylor R, Minor BL, et al.: The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019; 95: 103208. DOI: 10.1016/j.jbi.2019.103208. DOI: https://doi.org/10.1016/j.jbi.2019.103208
Wikipedia: List of medical schools in the United States. Available at https://en.wikipedia.org/wiki/List_of_medical_schools_in_the_United_States. Accessed September 25, 2023.
AAMC: 2022 physician specialty data report. Available at https://www.aamc.org/media/63371/download?attachment. Accessed September 25, 2023.
AAMC: 2021 state physician workforce data report. Available at https://www.aamc.org/data-reports/workforce/data/2021-state-profiles. Accessed September 25, 2023.
Franz B, Dhanani LY, Miller WC: Rural–urban differences in physician bias toward patients with opioid use disorder. Psychiatr Serv. 2021; 72(8): 874-879. DOI: 10.1176/appi.ps.202000529. DOI: https://doi.org/10.1176/appi.ps.202000529
Speerforck S: Reducing substance use stigma in health care. In Schomerus G (ed.): The Stigma of Substance Use Disorders. Cambridge: Cambridge University Press, 2022: 232-251, Chapter 13. DOI: https://doi.org/10.1017/9781108936972.013
Zanza C, Romenskaya T, Zuliani M, et al.: Acute traumatic pain in the emergency department. Diseases. 2023; 11(1): 45. DOI: 10.3390/diseases11010045. DOI: https://doi.org/10.3390/diseases11010045
National Institute on Drug Abuse: Words matter-terms to use and avoid when talking about addiction. Available at https://nida.nih.gov/nidamed-medical-health-professionals/healthprofessions-education/words-matter-terms-to-use-avoid-whentalking-about-addiction. Accessed September 25, 2023.
Crowne DP, Marlowe D: A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960; 24: 349-354. DOI: 10.1037/h0047358. DOI: https://doi.org/10.1037/h0047358
Wakeman SE, Pham-Kanter G, Donelan K: Attitudes, practices, and preparedness to care for patients with substance use disorder: Results from a survey of general internists. Subst Abus. 2016; 37(4): 635-641. DOI: 10.1080/08897077.2016.1187240. DOI: https://doi.org/10.1080/08897077.2016.1187240
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.










