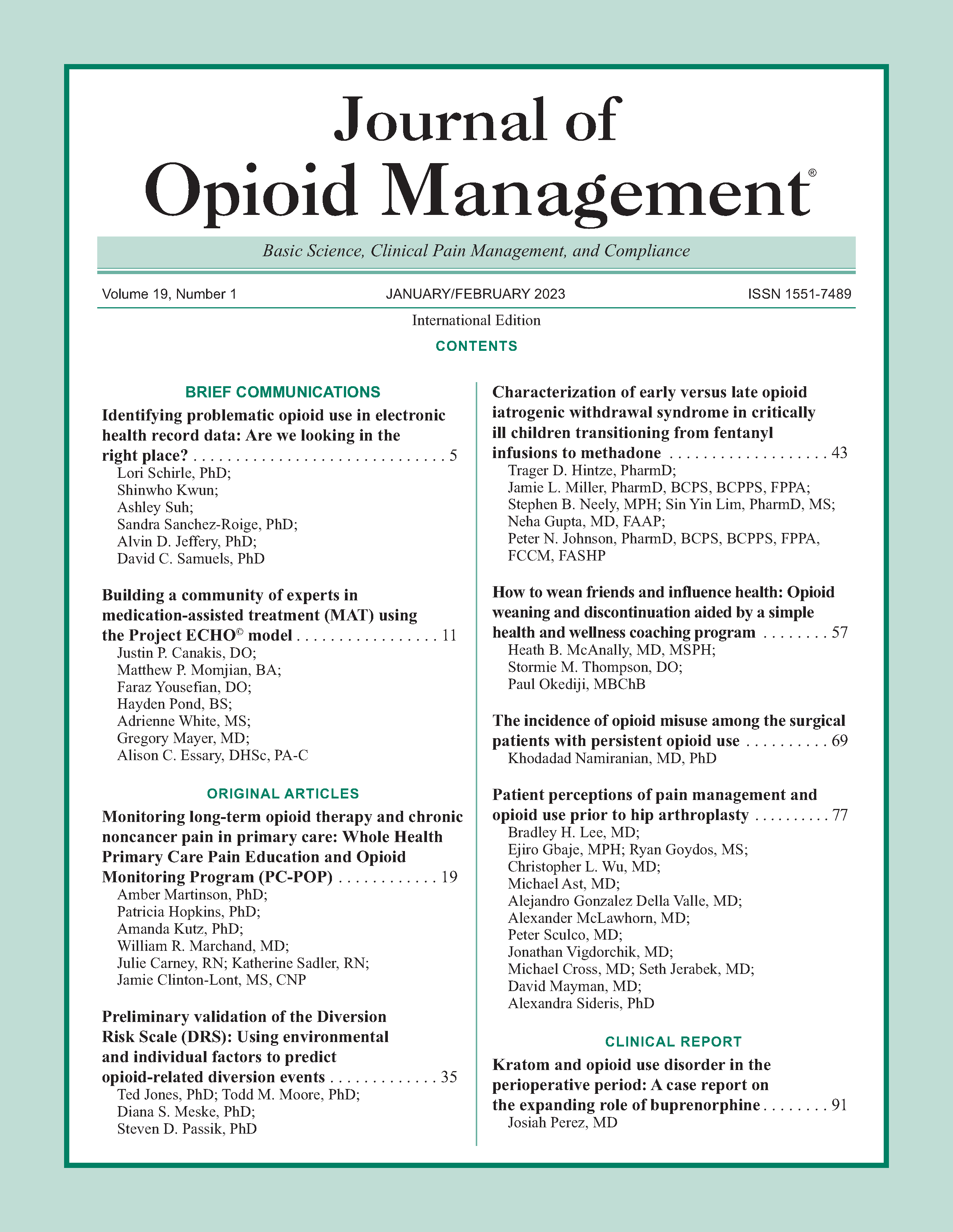
Patient perceptions of pain management and opioid use prior to hip arthroplasty
DOI:
https://doi.org/10.5055/jom.2023.0761Keywords:
patient education, opioids, pain managementAbstract
Objective: Qualitative assessment investigating patients’ perceptions related to opioids including their role in pain control, risks, and handling and disposal prior to undergoing hip replacement.
Design: A prospective, cross-sectional survey study.
Setting: Large urban teaching hospital specializing in orthopedic surgery affiliated with Weill Cornell Medical College.
Participants: Patients aged 18-80, English-speaking, without recent or chronic opioid use, and planning to undergo primary total hip replacement. A total of 128 patients were enrolled and completed the study.
Intervention: A 27-item interview evaluating perceptions on opioid-related topics.
Main outcome measures: Responses to interview questions were documented by research assistant.
Results: Most patients believe that there should be minimal or no pain with the use of opioids, though they also agree that opioids should be limited to pain that interferes with function or activity. Patients generally appreciate risks of addiction with opioids but are less familiar with risks associated with sleep apnea and sedatives. Minority of patients understand that the use of nonsteroidal anti-inflammatory drugs (NSAIDs) in combination with opioids would effectively reduce pain. Majority of patients were unsure of how to properly store and dispose of opioids.
Conclusions: Qualitative assessment demonstrates that patients may benefit from education and discussion specifically about pain expectations, the role of opioids in treating pain, multimodal analgesia, and proper storage and disposal.
References
Singh J, Yu S, Chen L, et al.: Rates of total joint replacement in the United States: Future projections to 2020-2040 using the national inpatient sample. J Rheumatol. 2019; 46: 1134-1140. DOI: 10.3899/jrheum.170990.
Roberts KC, Moser SE, Collins AC, et al.: Prescribing and consumption of opioids after primary, unilateral total hip and knee arthroplasty in opioid-naïve patients. J Arthroplasty. 2020; 35(4): 960-965.e1. DOI: 10.1016/j.arth.2019.08.036.
Sibia US, Mandelblatt AE, Caleb Alexander G, et al.: Opioid prescriptions after total joint arthroplasty. J Surg Orthop Adv. 2018; 27(3): 231-236.
Cook D, Kaskovich S, Pirkle S, et al.: Benchmarks of duration and magnitude of opioid consumption after total hip and knee arthroplasty: A database analysis of 69,368 patients. J Arthroplasty. 2019; 34(4): 638-644.e1.
Lee BH, Wu CL: Educating patients regarding pain management and safe opioid use after surgery: A narrative review. Anesth Analg. 2020; 130(3): 574-581.
Lemay CA, Lewis CG, Singh JA, et al.: Receipt of pain management information preoperatively is associated with improved functional gain after elective total joint arthroplasty. J Arthroplast. 2017; 32(6): 1763-1768. DOI: 10.1016/j.arth.2017.01.028.
Gangavalli A, Malige A, Terres G, et al.: Misuse of opioids in orthopaedic postoperative patients. J Orthop Trauma. 2017; 31(4): E103-E109. DOI: 10.1097/BOT.0000000000000741.
McCauley JL, Back SE, Brady KT: Pilot of a brief, web-based educational intervention targeting safe storage and disposal of prescription opioids. Addict Behav. 2013; 38(6): 2230-2235. DOI: 10.1016/j.addbeh.2013.01.019.
Nahhas C, Hannon C, Yang J, et al.: Education increases disposal of unused opioids after total joint arthroplasty: A cluster-randomized controlled trial. J Bone Joint Surg Am. 2020; 102(11): 953-960. DOI: 10.2106/JBJS.19.01166.
Syed UAM, Aleem AW, Wowkanech C, et al.: Neer award 2018: The effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: A prospective, randomized clinical trial. J Shoulder Elb Surg. 2018; 27(6): 962-967. DOI: 10.1016/j.jse.2018.02.039.
Stepan JG, Sacks HA, Verret CI, et al.: Standardized perioperative patient education decreases opioid use after hand surgery: A randomized controlled trial. Plast Reconstr Surg. 2021; 147(2): 409-418. DOI: 10.1097/PRS.0000000000007574.
Darnall BD, Ziadni MS, Krishnamurthy P, et al.: My surgical success: Effect of a digital behavioral pain medicine intervention on time to cessation after breast cancer surgery—A pilot randomized controlled clinical trial. Pain Med. 2019; 20(11): 2228-2237. DOI: 10.1093/pm/pnz094.
Sabesan VJ, Chatha K, Koen S, et al.: Innovative patient education and pain management protocols to achieve opioid-free shoulder arthroplasty. JSES Int. 2020; 4(2): 362-365. DOI: 10.1016/j.jseint.2020.01.005.
Bloom DA, Baron SL, Luthringer TA, et al.: Preoperative opioid education has no effect on opioid use in patients undergoing arthroscopic rotator cuff repair: A prospective, randomized clinical trial. J Am Acad Orthop Surg. 2021; 29: E961-E968. DOI: 10.5435/JAAOS-D-20-00594.
Berkwits M, Inui TS: Making use of qualitative research techniques. J Gen Intern Med. 1998; 13(3): 195-199. DOI: 10.1046/j.1525-1497.1998.00054.
Harris PA, Taylor R, Thielke R, et al.: Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42(2): 377-381.
Apfelbaum J, Chen C, Mehta S, et al.: Postoperative pain experience: Results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003; 97(2): 534-540.
Gan T, Habib A, Miller T, et al.: Incidence, patient satisfaction, and perceptions of post-surgical pain: Results from a US national survey. Curr Med Res Opin. 2014; 30(1): 149-160.
Elhage S, Thielen O, Huber A, et al.: Preoperative patient opioid education, standardization of prescriptions, and their impact on overall patient satisfaction. Surgery. 2021; 169(3): 655-659.
Horn A, Kaneshiro K, Tsui B: Preemptive and preventive pain psychoeducation and its potential application as a multimodal perioperative pain control option: A systematic review. Anesth Analg. 2020; 130(3): 559-573.
Wilder C, Miller S, Tiffany E, et al.: Risk factors for opioid overdose and awareness of overdose risk among veterans prescribed chronic opioids for addiction or pain. J Addict Dis. 2016; 35(1): 42-51.
Egan KG, De Souza M, Muenks E, et al.: Opioid consumption following breast surgery decreases with a brief educational intervention: A randomized, controlled trial. Ann Surg Oncol. 2020; 27(9): 3156-3162. DOI: 10.1245/s10434-020-08432-7.
Memtsoudis S, Poeran J, Zubizarreta N, et al.: Association of multimodal pain management strategies with perioperative outcomes and resource utilization: A population-based study. Anesthesiology. 2018; 128(5): 891-902.
Halawi MJ, Grant SA, Bolognesi M: Multimodal analgesia for total joint arthroplasty. Orthopedics. 2015; 38: 616-625.
Bicket MC, Long JJ, Pronovost PJ, et al.: Prescription opioid analgesics commonly unused after surgery: A systematic review. JAMA Surg. 2017; 152: 1066-1071.
Sabatino M, Kunkel S, Ramkumar D, et al.: Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg. 2018; 100(3): 180-188.
Neuman M, Bateman B, Wunsch H: Inappropriate opioid prescription after surgery. Lancet. 2019; 393(10): 1547-1557.
Published
How to Cite
Issue
Section
License
Copyright 2005-2025, Weston Medical Publishing, LLC and Journal of Opioid Management. All Rights Reserved.